Category: news
Unfortunately, even though the necessity for eight hours of sleep to wake up refreshed is widely recognized, the pressures of a hectic work schedule and modern living standards often result in people making do with … Read more
Unfortunately, even though the necessity for eight hours of sleep to wake up refreshed is widely recognized, the pressures of a hectic work schedule and modern living standards often result in people making do with just six hours. There’s a prevalent false belief that managing with six hours of sleep, along with regularly consuming double espressos, is enough to stay alert throughout the week. However, this is a major misunderstanding. A recent research on the effects of sleep deficit reveals that functioning on a mere six hours of sleep is tantamount to experiencing total sleep deprivation.

In the sleep deprivation study published in the Sleep Journal in 2004, 48 adult participants were divided into four groups. The first group was allowed to sleep for hours a night for two weeks. The second group was allowed to sleep six hours a night. The third group was allowed to have eight hours of sleep per night, and the fourth group was sleep deprived for three consecutive nights. The test subjects were also not allowed to take naps. Their cognitive performance, including their reaction time, mood and symptoms were monitored every two hours.
Not surprisingly, the group who slept eight hours each night had the best results. Test subjects who slept six hours a night did okay, but, as the end of the study was approaching (around day 10), their performance ratings got worse. The group who was allowed to sleep only four hours a night was getting worse each day.
The study found that the participants who slept only four or six hours a night had a severe decrease in cognitive performance. They were actually functioning the same as if they had been sleep deprived for two days. The only difference between the mentioned two groups was that the performance of the four-hour group declined much faster. Interesting information is that the participants that showed decreased cognitive performance after ten days of sleeping six hours per night were unaware of the changes based on their “sleepiness ratings”. This means that you hit the sack regularly for only six hours per night, you are not living your best life, and even worse, you may not even be aware of it. It’s time to back away from the Netflix, stop scrolling Instagram, and go to bed earlier.
Scientifically, sleep is understood as a distinct type of brain function, separate from wakefulness. During sleep, although brain cells function more slowly, they participate in profound and thorough activity. Sleep is a crucial component of your daily routine, claiming approximately one-third of your life. Ensuring you get quality sleep is equally important to following a healthy diet and consistently exercising.
Even though sleep is necessary for every individual, its biological purpose is still a mystery. Sleep affects almost every cell and system in the human body including the heart, brain, lungs, and body functions such as metabolism, and immune function. Scientific research shows that lack of sleep or poor quality sleep increases the risk of diseases such as diabetes, obesity, cardiovascular conditions, and high blood pressure. Sleep is a complicated and dynamic process that ultimately affects how human being functions, and scientists are finally starting to understand it.
What You Need to Know About Sleep Stages
Many people always think that not much goes on when one is sleeping in their bed. This is mainly because people who are sleeping usually look pretty peaceful irrespective of whether they are sleeping at night or during the day. Individuals may talk or even move during their sleep but it is mostly never meaningful or even purposeful. However, when it comes to sleep, there is more that goes on than what we imagine.
As you sleep, your brain will move through several different stages. Each of these stages will have different characteristics that may not be visible at the eye level but become more apparent when a sleeping individual is hooked up to some scientific measuring devices such as an EEG, a device that records the brain activity. Variations in the brain’s electrical activity will show whenever every stage of sleep starts and ends.

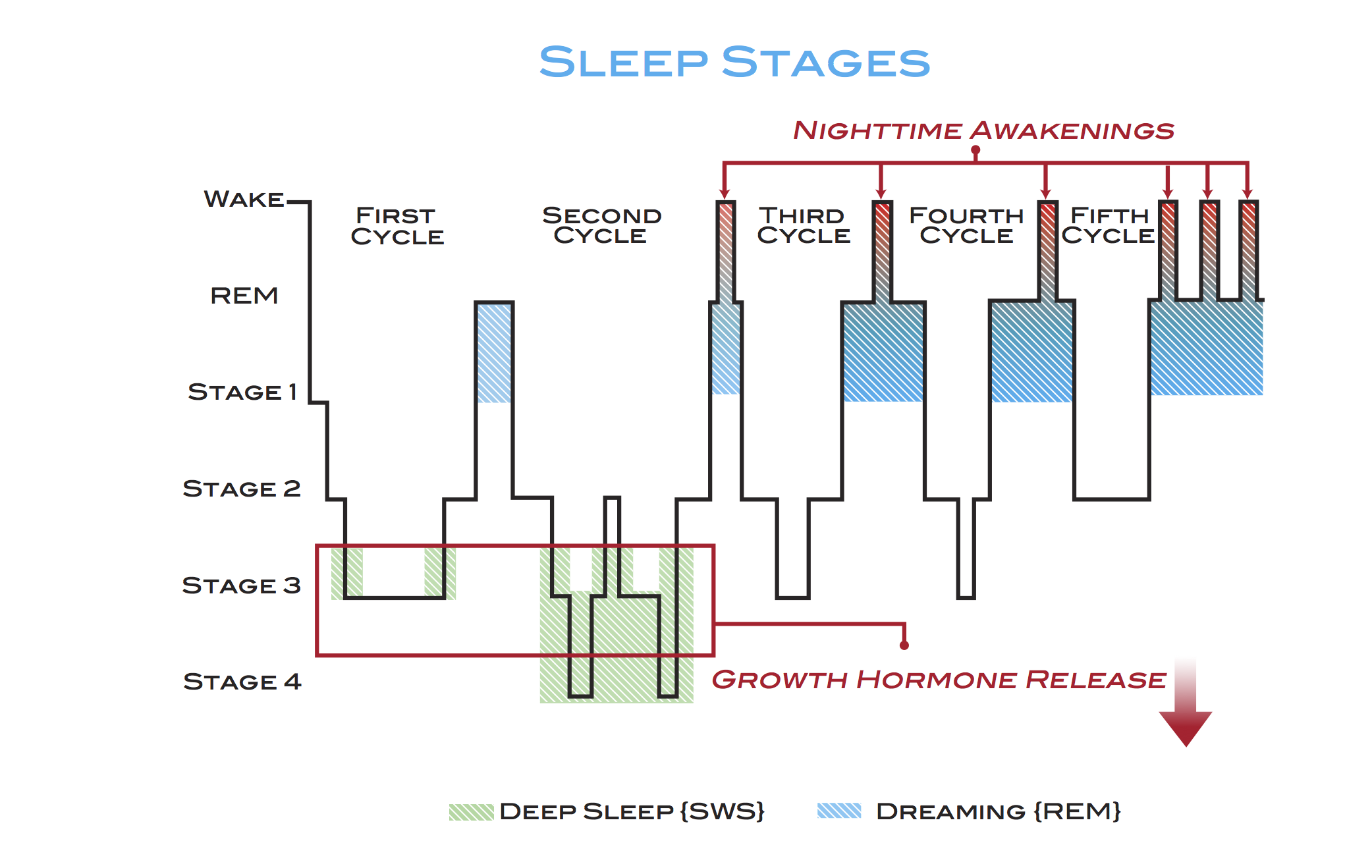
During the different sleep stages, there are also physical body changes such as muscular tension and changes in eye movement. Healthy people typically pass through five sleep stages – first, second, third, fourth and REM sleep stage. These stages always progress cyclically from stage one through REM and then begin again with stage one. An average complete sleep cycle takes from 90 to 110 minutes, and each stage can last from 5 to 15 minutes. The first sleep cycles typically have shorter rapid eye movement sleeps, and more extended periods of deep sleep. Later in the night, REM periods start to lengthen and deep sleep decreases. Even though you may not be aware of it, your body is always busy even when the mind is turned off.
STAGE 1
The first stage is light sleep, and it typically involves the act of falling asleep. You can feel extremely sleepy and may have challenges keeping your eyes open even for a minute. Additionally, your body may feel as though you are drifting in and out of sleep for some time. At this stage, you can be awakened even by the slightest noise and you will feel as though you have not got any rest.
At stage one, your body starts to prepare itself for deeper sleep. Your brain waves will begin to slow down, although they will look the same as when you were still awake. The breathing and heart rates will both go down, your muscles will relax, and your body temperature will start to fall. You will also become less aware of all external stimuli and your consciousness will start withdrawing from reality.
In stage one, many people experience something that can be described as the sensation of suddenly falling. This happens because the muscles are still active and they may suddenly contract. Every day you spend about 10% of your night in stage 1 or awake and some individuals tend to twitch at this stage. This first stage of sleep will usually last between 13 to 17 minutes. Basically, the first stage of sleep is when you fall asleep and it will only occur once during an uninterrupted night of sleep.
STAGE 2
Finding an exact line between stage 1 and stage 2 can be quite a challenge. However, stage 2 usually starts about 10 minutes after stage 1. In the second stage of sleep, eye movement completely stops and brain waves become significantly slower. This is the time when the body prepares for deep sleep. The body’s temperature slowly begins to decrease, muscles relax further, and your heart rate slows down. The electrical activity in your brain will occur at a lower frequency compared to when you are awake.
Most of your sleeping hours are spent in stage 2 as you cycle through all 5 stages several times through the entire night. Stage 2 will normally take about half of the total time that is spent sleeping. Waking up at this stage is pretty easy. However, it is not as easy when compared to stage 1. Stages 1 and 2 are usually referred to as the light-sleep phase. Together they usually last about 20 to 30 minutes.
STAGE 3
Stage 3 is the initial stage of deep sleep. In this stage, slow brain waves also known as delta waves become dispersed with smaller, faster waves. The shorter waves that tend to disappear as the sleep becomes deeper and deeper. Only in deep sleep, a person may experience parasomnias such as sleepwalking, night terrors, sleep talking, and bedwetting. Parasomnias typically occur during the transitions between non-REM and REM sleep.
Your breathing and heartbeat slow down to the lowest level during this stage and the muscles are completely relaxed. It is incredibly challenging to wake up stage 3 sleepers and they may not respond to noises of even 100 decibels. Waking someone at this stage is like trying to wake up an animal that is hibernating in the middle of winter. When they wake up at this stage, they will be confused, disoriented, and groggy.
People tend to reach stage 3 about 20 to 30 minutes after they start sleeping. At this stage, you are completely disconnected from reality. Stage three is one of the most restful parts of your sleep every night.
STAGE 4
Stage 4 of sleep is basically a deeper extension of stage 3. Deep sleep continues, and the brain produces more delta waves than in stage 3. The difference between these two stages is the fact that stage 4 is usually characterized by longer and slower delta waves in the brain. At this stage, the body is usually slowed down than ever before. The breathing and heart rates are substantially different from what they actually are during the day. Individuals who have any sleep disturbances will start experiencing them as the body transitions from stage 4 into the REM sleep. In case you are awakened from this state, you will feel very disoriented for a few minutes.
Stage 4 of sleep usually starts approximately 45 minutes after you start sleeping. Stages 3 and 4 are called the deep-sleep phase and they usually constitute about 20% of the entire sleeping time. However, this proportion tends to decrease as one gets older.
REM Sleep Characteristics
The REM sleep cycle begins at least 80 to 100 minutes after you fall asleep. The deep-sleep phase ends abruptly and this is usually accompanied by a change in the sleeping position. The sleeping individual will switch back to stage 2 for several minutes before the EEG graph shows an abrupt change within a span of a few seconds. This is an indication of the REM sleep stage beginning.
In REM sleep, your brain waves activity is very similar to the activity in the state of wakefulness. The eyes are closed but more rapidly from side to side. This is the stage when intense dreaming occurs. Only 20% of the entire sleeping hours are spent on this stage. This percentage tends to be significantly higher in small children and infants.
When healthy individuals are in a state of REM sleep, their body muscles are deeply relaxed. If the muscles were not relaxed, those people may act out their dreams and this can have severe consequences. This is the main reason why the brain will put the body in this deep state of relaxation that is known as astonia and it borders close to paralysis. However, individuals who suffer from medical conditions, for example, Parkinson’s disease do not experience REM astonia and as a result, they can act out their dreams.
Why is REM Sleep Important?
Of all the sleep stages, however, the REM stage seems to have the most fascinating benefits. Just like the deep sleep stage, REM sleep has a healing power – experts say that REM sleep is a restorative stage where the body gets to heal itself.
REM sleep stimulates the brain – especially for children, REM sleep is vital in stimulating areas of their little brains. This brain stimulation is very important in retaining memories and also recording and learning new things. Just like deep sleep, REM sleep boosts the production of proteins. Scientists have approved that protein synthesis happens when the body is in sleep mode; something that is highly beneficial for muscle and overall body growth. Old or young, we all need to grow and develop our muscles.
REM sleep has been associated with pain relief – believe it or not, patients who, say, have a leg injury and get good sleep sessions will get some pain relief, while those that do not get REM sleep at all will often complain of the pain worsening, especially during the night.
| WAKING | REM SLEEP | NREM SLEEP | |||
| Stage 0 | Stage R | LIGHT SLEEP | DEEP SLEEP | ||
| Stage 1 | Stage 2 | Stage 3 | Stage 4 | ||
| Eyes are open, and responsive to all types of external stimuli. The person can hold comprehensible conversation. | Brain waves are very similar to the state of wakefulness. Most vivid dreams happen in stage R. Body does not move. | Transition between waking and sleep. When awakened in this stage, a person will claim the never fell asleep. | Main stage of light sleep. In this cycle memory consolidation and synaptic pruning occurs. | Slow brain waves on EEG readings. | Slow brain waves on EEG readings. |
| 16 to 18 hours per day | 90 to 120 min/night | 4 to 7 hours per night | |||
What Is a Sleep Cycle?
A sleep cycle is a period of time required to go through the 5 stages of sleep explained above. It’s a very interesting fact that we don’t have to transition from deep sleep to rapid eye movement right away. During a sleep cycle, we can go through the stages of non-REM sleep. For example, you can go through light and deep sleep, and then reverse back from deep to light sleep, and end your sleep cycle in REM sleep. Of course, in order to wake up naturally, you have to go into the stage of light sleep. When you go back into light sleep, you don’t have to wake up necessarily, you have just completed one full cycle, and as mentioned above, a person goes through one than one sleep cycle per night. Once you have fallen asleep, you will be longer in deep sleep than in REM sleep. However, as the night progresses, you will spend more time in REM sleep and less in deep sleep.
It’s an interesting fact that sleep quality tends to change with the transition from one stage of sleep to another. Every transition of sleep is marked by subtle variations in bodily functions and every stage is part of a predictable cycle whose intervals can be observed. Sleep stages can be examined and monitored clinically using polysomnography that provides information about muscular and electrical states during sleep.
The Purpose of Sleep Cycles
Every sleep phase has specific purposes for the body. The main function of both light-sleep and deep-sleep is rejuvenating and restoring the body and the mind. During the REM stage of sleep, the brain is usually just as active as it is when one is awake. For you to process the memories and experiences of the previous day, both REM sleep and deep sleep are important.
The brain uses sleep time to weigh up the information that you have absorbed during the day while you were awake and to organize your memories. Additionally, the brain will also store any crucial information in the long-term memory and discard some other details and information. This is the main reason why having a good night’s sleep is important for your focus, memory and concentration.
How Long Is a Sleep Cycle?
The length of a sleep cycle can vary from person to person. Typically, a sleep cycle lasts from 90 to 120 minutes. The first cycle usually lasts around 90 minutes. After that, the sequences extend a bit and last from 100 to 120 minutes. A healthy individual goes through four to five sleep cycles a night.
What Is The Deepest Stage of Sleep?
The third and fourth stage of sleep is known as deep sleep. Deep sleep can also be called slow wave or delta sleep. It’s very difficult to wake up someone from stage 3 and stage 4. Children are nearly impossible to wake up from deep sleep, and in this stage, parasomnias such as night terrors, sleepwalking, sleep talking, and bedwetting may occur. In stage 3 and 4, there is no eye movement or muscle activity.
Deep sleep provides the most restorative sleep of all the sleep stages. This is why taking a short nap during the day probably won’t affect your ability to fall asleep at night. However, if you nap for too long and transition into deep sleep, you will have more difficulties hitting the hay at night. Deep sleep reduces your need for rest.
In delta sleep, human growth hormone is released which helps to restore your muscles and body. Your immune system also restores itself. Lastly, our body and mind refresh themselves for new experiences and learning the following day.
When Does REM Sleep Occur?
Deep sleep comes in the first half of the night, therefore, REM comes in the second half. This stage typically begins about 90 minutes after you first fall asleep, and the first cycle only lasts for 10 minutes. As the night progresses, REM cycles will become longer, and the last rapid eye movement will last up to one hour. Most healthy people experience 3 to 5 stages of REM sleep per night.
After REM sleep you transition into light sleep, therefore it may be possible to wake up. However, even if you wake up, you probably won’t remember it. Only if the waking period is long enough, you may remember it in the morning.
In REM sleep, brain waves in this stage are very similar to the ones in a state of wakefulness. During this sleep cycle, your breathing will become faster, irregular and shallow; your eyes will jerk rapidly, and your limb muscles will be paralyzed temporarily. Your heart rate increases and blood pressure rises. Males may develop erections. Lastly, your body loses some of the ability to regulate temperature.
When Do We Dream?
The brain is most active in REM sleep, therefore, this is the time most vivid dreams occur. When someone is awakened during rapid eye movement, he or she can remember their dream. REM stage is followed by temporary muscle paralysis. Many scientists believe this is a form of protection from acting out our dreams. Individuals who suffer from REM sleep behavior disorder, don’t experience this temporary muscle paralysis and therefore acts out their dreams. Even though most us don’t remember it, studies show that we all dream multiple times a night. A person dreams around 4 to 6 times every night.
Brain Waves During Sleep
Sleep research is still a relatively new and young field. An interesting fact is that scientists discovered REM in the middle of the twentieth century when new machines for monitoring brain activity were developed. Before this, scientists believed that sleep was a rather passive state when all brain activity ceased. Since 1953, researchers have disproved the idea lack of REM sleep leads to insanity. On the contrary, they actually found out that REM sleep can relieve the symptoms of clinical depression. New studies link REM sleep to learning and memory.
Does Sleep Cycle Change with Age?
The amount of time you spend in each stage of sleep depends on your age. Infants spend almost 50% of their time in REM sleep, while 50% of adults spend half of their sleep time in light sleep. 20% of adults spend most of their sleep time in REM. Older adults spend significantly less time in REM sleep, and that amount of time further decreases as they age.
Sleep Cycle in Babies and Children
The cycles of deep and light sleep in babies usually lasts about 30 to 50 minutes and then increases gradually in length across childhood. Some infants and children tend to fall deeply asleep quite quickly. Other children will sleep lightly while muttering and fidgeting for at least 20 minutes before they actually get into deep sleep.

Children normally wake up briefly before the end of every sleep cycle. All children do this because it is a customary part of healthy sleep. Some kids may even call out when they wake up at night and they will require assistance settling again. However, individual sleepers usually put themselves back to sleep. Not all parents will hear their children when they wake up at night.
Sleep Cycle in Adolescents and Adults
In adolescents and adults, every sleep cycle will end in a brief awakening and this can occur several times throughout the night. These awakenings do not usually interfere with our sleep and most times, we are not aware of them. If things do not change, then we will most likely go straight back to sleep. However, if anything changes around us, for example, if the pillow is missing, you feel anxious or uncomfortable, or you are disturbed by any noise, then one may wake up fully.
Factors that Affect Sleep Cycles
The sleep cycle is quite variable and it can be influenced by different agents. Sleep cycles, duration, quality, and the onset of sleep can be affected by sleep disorders. Additionally, the progression of sleep cycle can also be affected by sleep deprivation, stress, environment, and changing sleeping schedules frequently. A sleep disorder such as narcolepsy can affect the time it takes a person to achieve the rapid eye movement latency.
Psychological conditions such as depression can also shorten the length of the rapid eye movement sleep stage. Treatment modalities for psychiatric conditions also affect sleep in patients and can also induce a change in their sleeping habits. For example, the use of antidepressants such as Prozac can cause insomnia and trouble sleeping, and can also inhibit REM sleep stages.
A lot of people think of sleep as a time when both the mind and body enter a shutdown mode. However, this view doesn’t reflect reality. Actually, sleep is an active period during which vital … Read more
A lot of people think of sleep as a time when both the mind and body enter a shutdown mode. However, this view doesn’t reflect reality. Actually, sleep is an active period during which vital strengthening, rejuvenation, and important processing tasks occur.
Why the body is programmed for extensive periods of slumber and how the process happens is still a bit of a mystery. However, scientists are aware of some of the critical functions of sleep and why it is necessary for the optimal well-being and general health.
Roles of Sleep
Consolidating and solidifying memories is among the critical roles of sleep. While going about your day, the brain consumes an astonishing amount of information. Instead of being logged in and recorded directly, these experiences and facts need to be processed first and then stored. Many of these functions or steps take place as you sleep.
Pieces and bits of information are moved from more short-term and tentative memory to long-term, stronger memory overnight during a process that is known as consolidation. Research also shows that after sleeping, people tend to perform better during memory tasks and retain information. All bodies need substantial periods of sleep for the purpose of synthesizing hormones, repairing tissue, growing muscle, rejuvenation, and restoration.
Healthy Sleep for Everyone
Healthy sleep is important for everyone because we are all expected to learn skills to develop in life and retain information. However, this is probably part of why children who acquire motor, social and language skills at a rapid pace during their development require more sleep than adults do.
Adults typically require 7-9 hours of sleep each night while young children need 9-11 hours and teenagers thrive with 8-10 hours of sleep. During the vital periods of learning and growth, young people require a large dose of sleep for optimal alertness and development.
Sleep Habits
Unfortunately, an individual cannot be sleep deprived and make up for it by logging several hours of slumber, even though repaying so-called sleep debt can be a good idea in case you have accumulated sleep deprivation. Good sleep habits are healthy, consistent routines that enable everyone, regardless of their age, to fulfill their sleep needs each night and handle the challenges of daily life.
Sleep in a Nutshell
- The body regulates sleep in the same way it regulates breathing, drinking and eating. This indicates that sleep plays a similar crucial role in your wellbeing and health.
- While it can be challenging to address the issue of ‘why sleep is necessary’, several theories have been developed by scientists to explain why a third of people’s lives are spent sleeping.
- Being aware of these theories helps to give insight into the function of sleep and why it matters.
Sleepiness and Hunger
Although people may not think about the reasons for sleep often, many of us realize that sleeping enhances how we feel at some level. You feel happier, more energetic and more alert and have the ability to function better after a good night of sleep. But the fact is that slumber makes you feel better and going without it makes you feel worse is only the beginning of explaining and understanding the necessity of sleep.
- One of the ways to consider the role of sleep is by comparing its other activities that are necessary for sustaining life such as eating. Hunger serves as a protective mechanism that ensures you consume the food and nutrients your body needs to function properly, repair tissue and grow.
- Although it is fairly easy to understand the role of eating, since it consists of consuming substances physically to meet your body’s needs, sleeping and eating are not as different as they might appear to be.
- Both sleeping and eating are regulated by internal, powerful drives. An unpleasant sensation of hunger results from going without food while lack of sleep makes you feel extremely sleepy. Just like eating easing hunger and makes sure that you get the nutrients you need, sleeping eases sleepiness and makes sure that you get the sleep you need.
- The question still remains regarding whether or not we need sleep and whether there is one main function of sleep or if it serves several functions.
Answering the Questions
Scientists continue to explore the issue of sleep’s importance from several different angles. For example, they have examined what occurs when animals and humans are deprived of sleep. Other studies have observed sleep patterns in various organisms to find out whether differences or similarities among species can reveal things about the functions of sleep. Despite many years of research and several discoveries about various aspects of sleep, it has been difficult to answer the question of why sleep is necessary.
Theories of Sleep
Lack of clarity or a clear answer to the question does not suggest that research has been pointless. In fact, much more is known about the role of sleep and scientists have been able to develop many promising theories that explain the reasons for sleep.
Considering all the evidence that has been gathered so far, a single theory may not be proven correct. Rather, sleep may be explained by a number of these explanations. The goal is to have an in-depth understanding of why we sleep and learn to appreciate the role of sleep more while enjoying the health benefits it provides.
What Sleep does
Human beings spend almost a third of their lives sleeping. Lack of sleeping can disrupt your mental health and even have fatal consequences. It is clear that getting enough shut-eye is vital for your body to function. However, what sleep does is still an unsolved mystery. For example, why we need to eat is obvious but why we need to sleep is unclear.
People are vulnerable while sleeping and the function of sleep must be worthwhile in order to take the risk of keeping the brain offline during this period. There are a number of theories regarding sleep and while none of them are completely solid, some of them attempt to explain what occurs each night with research about topics that range from cognition to cellular processes. Researchers say that sleep is clearly the key to the ability of the brain to reorganize, a characteristic that is known as plasticity.
Stages of Sleep
Proving that sleep is crucial is not hard. Published studies have found that an entire day of sleep deprivation can cause healthy individuals to have schizophrenia problems such as hallucinations. Since sleep is actually hard to study and isolate, delving into why we sleep can be difficult.
- Studies on sleep deprivation are a common way to explore sleep. However, being deprived of sleep interferes with several biological systems, which makes it difficult to determine the outcomes that can be directly linked to sleep deprivation instead of stress, for example. The biology of the brain in the different stages of sleep is another reason that makes it hard to understand sleep.
- Sleepers go through a cycle of non-REM or non-rapid eye movement and REM or rapid eye movement sleep as the night goes on. Studies show differences in the brain’s biology during different stages of sleep. For instance, growth hormones are released during non rapid eye movement sleep.
- Some genes that are involved in synthesizing the proteins of the body are more active. In contrast, there does not seem to be an increase in this type of activity during rapid eye movement sleep.
Information about Sleep
One of the conclusions that have emerged is that sleep seems to be primarily a phenomenon that is focused on the brain. While being deprived of sleep changes hormone levels within the body and has an impact on the immune system, its impact is most consistent in the brain.
The central nervous system is often affected by sleep. Other things may have been added to the main function of sleep by evolution but the main function of sleep is likely to be something that is associated with the brain.
What goes on during Sleep?
One of the theories that have been developed by scientists is that the brain’s energy is restored by sleep. If the concept of sleep restoring brain energy is accurate, the relationship between the use of brain energy and sleep is not straightforward. More research is necessary to understand this connection.
Another concept is that sleep may allow the brain to get rid of toxic products that are generated when we are awake. Brains consume a lot of energy and subsequently produce a lot of waste. Sleep can be a time when brains are cleaned out. This may be something that occurs during sleep but it may not necessarily be the most essential thing that sleep does.
Plasticity and Connectivity
The most convincing theory regarding sleep may be that plays a key role in the plasticity and connectivity of the brain.
- Plasticity is an aspect of memory and learning. While it is not exactly clear how this works, evidence seems to suggest that lack of sleep can lead to problems with memory, especially working memory that enables people to retain information in an accessible way while dealing with a problem. Individuals who are sleep deprived also find it hard to regulate their emotions and choose what they should pay attention to.
- The impact of sleep on plasticity may be seen through its influences on the connection between neurons, otherwise known as the synapses. This could mean that there is something central and basic at the core of sleep in reference to a basic function of the brain cells that can result in plastic change.
- A better comprehension of sleep in the future may be yielded from further research o the brain cells, including those that were previously thought to be inert. Understanding what certain specialized cells do may help to solve the mystery of sleep.
Basic Human Need
- Sleep is a basic human need with a third of people’s lives being spent on it and dire health consequences of sleep deprivation. Sleep is as essential as water and food, which is why there is an ongoing need to understand why we spend so much time doing it.
- One of the main reasons that have been cited for sleep is because people get sleepy. Since the ancestors were susceptible to attacks while lying unconscious for long periods of time, researchers say there must be a number of advantages that outweigh this significant risk.
- The main hurdle in comprehending the purpose of sleep was the hidden nature of brain activity that happens during sleep. New methods have helped researchers understand the function of sleep better.
Researching the Brain
Additional evidence shows that sleep enables you to consolidate memories. This is an important process that converts short-term memory into long=term memory.
- While sleeping, the brain consolidates information that has been gathered in a day through the opening of pathways within the pyramidal neurons. This process along with reorganizing the network takes time and can only happen when processes like sensory processing do not occur. Consequently, this may be the ultimate reason why sleep is necessary.
- Some researchers have noted that the benefits of consolidating our memories do not necessarily outweigh the risks that are associated with sleep. They point to other theories instead. Suggestions include sleep giving the brain a vital chance to get rid of trash.
- In published studies, researchers discovered that cerebral spinal fluid clears waste chemicals by being pushed around the brain to eliminate what has been generated as a result of natural cell activity. This waste removal method mainly happens during sleep, which is comparable to a party with the option of either entertaining your guests or cleaning up since you cannot practically do these tasks at the same time.
Energy Demands and Expenditure
Another theory about why we sleep suggests that sleep is linked t energy demands. This is a theory that is based on natural selection. Since the availability of prey and animal performance peak at varying times of the day, sleep may have been chosen as a way to save energy.
However, this theory may be flawed because it does not adequately explain choosing REM sleep that increases energy expenditure in most species. Inevitably, all the primary theories have limitations in an attempt to solve the mystery of sleep but advancements in technology and ongoing interest in the issue can produce the definitive answer that has been elusive for a long time.
Insight into Sleep
Sleep is an essential and indeed normal part of life but when you think about it, it seems to be an odd thing to do. As each day ends, people become paralyzed and unconscious. Sleep made the ancestors susceptible to being attacked by wild animals.
This means that the potential risks of the process that is universal among various groups, including mammals, must provide some type of evolutionary benefit. Research within this area has slowly taken off. But there has been a recent surge of intriguing revelations that give researchers new insight into the reasons for sleep and answers to the question ‘why do we sleep’.
- Scientists have seemingly been reluctant to give a conclusive explanation of why we sleep. Broadly, researchers believe that sleep allows the body and particularly the brain to recover. Researchers have recently found out more about the detailed aspects of the processes involved.
- Brain cells establish connections with different parts of the brain during the day due to new experiences. It seems that vital connections are strengthened while unimportant ones are extracted during sleep. Experiments performed on sleep-deprived animals like rats show that the process of strengthening and purging mainly happens when they are asleep.
- Sleep is also a chance to clear the brain of waste.
Effects of not getting enough sleep
- Lack of sleep seems to change the way that the genes within the cells of the body behave. Researchers have found that the genes that participate in inflammation appear to increase their activity. The genes respond to sleep deprivation as if the body is stressed.
- Speculations revolve around past times when ancestors’ bodies were prepared for injury through the activation of inflammation genes that cushion the impact of attacks by human enemies or wild animals. The body is placed on alert for wounds but the wounds do not occur. This can easily help to describe the relationship that exists between negative health consequences and lack of sleep like stroke and heart disease.
- However, preparing for injuries that do not occur does not have a beneficial effect in modern times. In fact, activating the immune system may heighten the risk of stroke and heart disease.
Why is it harder to think when you are Sleep Deprived?
Half asleep is an expression that might accurately describe what goes on inside the brain when you feel tired. Research shows that components of the human brain may actually be asleep due to lack of sleep. Studies on dolphins and whales show that when they sleep, they continue using a portion of the brain to rise to the surface for air and swim.
Studies on human patients reveal that the same thing goes on in the brain. While their sleep deprivation increases, components of their brain become inactive even when they are still awake. Additionally, local areas of sleep move around the brain. Even when you go to bed and think that you are awake at one moment, there is an abrupt alteration of sleep; it may actually be a continuous process.
Purpose of Dreaming
Psychiatrists have attempted to answer the question regarding the role of dreams and their success may be regarded as limited. Devices have been created for the purpose of reading or understanding dreams and serve as a worthwhile step towards seeing more details of what occurs in dreams and enable researchers to learn more about the reasons for dreaming.
Impact of Modern Life on Sleep
Many studies show how electricity has led to people altering their days and ending up with less sleep. People go to bed and awaken a couple of hours later on average in comparison to past generations. Working adults, including shift workers, are well-known for getting less than six hours of sleep each night.
Reading electronic books prior to going to bed can make it harder to fall asleep, which leads to lower levels of the hormone that controls the internal clock of the body and makes you less alert the following day.
Over the years, there has been a notable decline in the quality and duration of sleep. Since many people are opting for electronic devices that they use for entertainment, communication and reading, especially adolescents and children who already experience a substantial amount of loss of sleep, research that can evaluate the long-term effects of these devices on safety and health are urgently required.
What prevents Sleeping?
- Keeping mobile devices turned in bedrooms at night can increase the risk of disrupting your sleep. Consuming red wine and foods such as nuts, cheese and bacon may also keep you up at night.
- Several studies show evidence that loss of sleep is linked to lower life expectancy, diabetes, and obesity while others believe that these types of assessments instill unnecessary fear in people.
Sleep and Health
Sleep is important and it is as essential to the body as breathing, drinking and eating along with being crucial for maintaining good physical and mental health. Sleeping enables you to recover from physical as well as mental exertion. There is a strong relationship between health and sleep as poor sleep may increase the risk of poor health that can exacerbate the problem of finding it hard to sleep.
- One of the signs of distress may be sleep disturbances. Common mental health issues such as depression and anxiety can often amplify sleep problems. Exploring the mental health and sleep within the realm of mental health awareness helps to show the effect of sleep on mental wellbeing.
- Everyone is aware about the myth of getting out of bed and pulling yourself together but disturbed sleep, tiredness, and lethargy can be an aspect of mental health issues or a side effect of medication. Dealing with sleep disorders and sleep as a component of treating mental health is very crucial and can easily be overlooked.
- Sleep can be particularly challenging in work that is based on shift and in industries that are critical in terms of safety such as the railways sector. This is why it is even more essential to ensure that you get a sufficient amount of quality sleep.
- Everyone can benefit from enhancing the quality of their sleep. For most people, it may be a case of attitude changes or making small lifestyle changes to help them sleep better. As much as a third of the entire population might suffer from poor quality sleep, lack of sleep, insomnia, and other sleep problems.
- Lack of sleep can affect the ability to function and stay awake at work during the day, concentration levels, energy, mood, and relationships.
Basic Techniques and Treatment
There are basic techniques that can help to improve your sleep. Speaking to your doctor about possible treatment solutions is important if these techniques do not work, especially since sleep problems may be an indication of other health issues. Persistent sleep problems may mean there is an underlying issue that needs to be discussed with a health professional. Treatment for sleep problems along with mental health issues can be useful for addressing both the signs and causes in order to speed up recovery.
There are a number of things that need to be considered when dealing with poor sleep or sleep deprivation.
Health
It is well known that lack of quality sleep can affect sleep. Mental health issues such as anxiety and depression are often associated with sleep problems. It is essential to make sure that all health concerns are dealt with to ease physical symptoms and address the worries that may be keeping you awake.
Surroundings
Wherever you sleep is vital and the bed and bedroom should primarily be places that are associated with sleep. Eating in bed, playing with screens or phones or watching television can all have an effect on the overall quality of sleep. Light, noise levels and temperature all play a role in determining the kind of sleep you get. If you experience poor sleep, you can consider creating a sleep diary that shows whether there are patterns that can help you identify the problem.
Attitude
It is easier to fall asleep when you let go of worries and are able to relax. Everyone has had a night that involves lying awake and worrying. During the time before going to bed, it is important to wind down, relax and minimize stimulation. It can be hard to do this these days but a warm bath and relaxation techniques are some of the things that can help.
If you find it hard to sleep, you can get up and prepare a warm drink of milk, for example, and make another attempt to get to sleep when you feel sleepier. Turning on the phone screen or TV may be tempting but this might stimulate you and falling asleep becomes harder.
Lifestyle
What you drink and eat can influence your sleep.
- Stimulants such as caffeine can make it difficult to sleep and a sugary or heavy meal just before bed can disrupt sleep or make it uncomfortable.
- Alcohol may seem to make you sleepier but it diminishes the actual quality of sleep.
- Exercising during the day is another good way to promote better sleep but exercised during the evening or at night may not be helpful since they release adrenaline.
Reasons to Get Sufficient Sleep
Many people are not getting as much sleep as they need and a large percentage of people experience sleep difficulties at least some nights each week. Insomnia on a short-term basis may not be something to worry about.
A major concern is chronic loss of sleep that can lead to health problems like weakening the immune system, high blood pressure and weight gain. Although more research is required to explore the relationship between health and chronic loss of sleep, it is safe to conclude that sleep is too essential to ignore.
- Memory and learning- Sleep enables the brain to gather new information and commit it to memory through a process that is known as consolidation. Studies have shown that people who get enough sleep after learning a new task are more likely to perform better on tests in comparison to those who do not.
- Weight and metabolism- Ongoing sleep deprivation can lead to weight gain because it affects how your body processes and stores carbohydrates as well as altering the hormone levels that affect your appetite.
- Safety-Lack of sleep contributes to a higher tendency of falling asleep during the day. These lapses can lead to falls and errors such as road accidents, air traffic mishaps, and medical mistakes.
- Mood- Loss of sleep may result in moodiness, lack of ability to concentrate, impatience and irritability. Poor sleep can also make you too tired to accomplish the things you want to do.
- Cardiovascular health- Major sleep disorders are linked to irregular heartbeat, an increase in the levels of stress hormones and hypertension.
- Disease- Being sleep deprived can alter the immune function, which includes the activity of body cells.
- Getting enough sleep can help to fight serious medical conditions such as cancer.
Conclusion
A good night of sleep is very important for your health, just as crucial as exercising and eating healthy. Unfortunately, modern life and lifestyles have interfered with sleep patterns. People sleep less than they did and there has been a significant decline in the quality of sleep.
Good sleep is necessary for the following reasons:
- Lack of sleep can make you gain weight.
- Good sleep can help you consume fewer calories.
- Good sleepers generally have better concentration and are more productive.
- Quality sleep can improve athletic performance.
- Lack of sleep increases the risk of stroke and heart disease.
- Sleep has an impact on the risk of Type 2 diabetes and glucose metabolism. Sleep deprivation is associated with depression.
- Sleep strengthens your immune system. Loss of sleep has been linked to inflammation. Sleep affects social interactions and emotions.
- Along with exercise and nutrition, good, quality sleep is among the essential pillars of good health. It is virtually impossible to be optimally healthy if you do not prioritize your sleep and take proper care of it.
The objective when we go to bed is to attain a state of slumber that rejuvenates us, making us ready for the upcoming day. However, this objective can be hard to achieve due to various sleep disorders that may disrupt our nightly rest. These issues can vary greatly in both their intensity and symptoms. For those suffering from such conditions, the result is often sleep that is neither tranquil nor rejuvenating as hoped.
Importance of A Good Night’s Sleep
If you are having trouble sleeping at night, you need to deal with the problem causing the sleep-related issue as soon as you can. This is because sleeping is important for the overall functioning of your body. When you are not getting adequate sleep, you will find yourself suffering from other health issues that will affect how you live your life.
Experts recommend at least 7 to 8 hours of sleep every night, which becomes impossible when you have something interrupting it. The recommended hours of sleep give your body adequate rest while allowing other body functions to happen when you have shut down. When you are awake, many activities are taking place. Your mind is receiving information, your muscles are in use and you are eating every other time.
Sleep allows some of your body systems time to rest, and others to work without interruption. You stand to gain the following benefits that lead to good health when you are getting adequate sleep.
- Improved brain function
Adequate sleep ensures that the brain functions at its best always. While you rest, your brain carries out the consolidation process, which is vital and leads to strengthening of the memory. This process makes it easy to learn a new skill. Brain functions that support cognition, concentration and even performance become better with adequate sleep. When you are sleep-deprived because of sleep-related disorders, you are bound to make mistakes. Such mistakes can endanger your life and that of others such as when you cause an accident.
- Better digestion
While you sleep, your digestive system gets time to process the ingested food. The system works well as you rest as it has time to process the food in the system without interruption. As you are not eating while you sleep, the body gets to clear the food. When you do not give the body time to do this, the risk of getting inflammatory disorders of the stomach is high. Such disorders get worse or recur after treatment if you get few hours of sleep every night.
- Improved cardiac function
Adequate sleep helps to minimize the presence of inflammatory proteins in the blood. These inflammatory proteins cause heart diseases that can lead to heart attacks and high blood pressure. Studies indicate that less than seven hours of sleep increases the risk of heart attacks. The only way to avoid this is to ensure adequate sleep. This can become hard when you are battling sleep disorders of any type such as restless legs syndrome (RLS).
- Lower incidence of diseases
You will have a stronger immune system when you sleep well. This means that you will have lower risk of getting diseases such as the common cold. Suffering from sleep disorders hinders your body’s ability to fight diseases. The significant boost of the immune system function through adequate sleep sees you enjoy a good quality of life with minimal disruptions to your lifestyle due to poor health. You also have better management of your blood sugar levels, thus keeping diseases such as Type 2 diabetes at bay. Studies also show that getting good sleep helps patients have a better handle on arthritis. You even maintain young looks for longer.
- Maintenance of healthy body weight
Sleep supports the function of the body that regulates hormones. Some of the hormones regulated include those that affect appetite. When your body gets enough rest, the levels of hormones that increase the desire for food are at healthy levels, and so are those for the hormones that suppress appetite. When the body gets only a few hours of sleep, the body has increased levels of appetite-stimulating hormones, which increase your chances of being obese. On the same note, by sleeping well while on diet, you see increased loss of fat as opposed to loss of muscle mass when you’re not getting enough sleep.
- Improved mental health
Sleep deprivation due to sleeping disorders does not go well for those with mental health issues. Studies show that stress levels are high when the body does not get enough rest. People who suffer from conditions such as depression, ADHD and such other issues see their situations worsen when they do not get enough sleep. Even if you do not suffer from any mental issues, you will have better social interactions when you sleep well as you have improved the ability to read emotions better. Sleep, therefore, is an important factor and when sleep disorders disrupt it, you are open to many risks, which affect various areas of your life. You will be more productive at work, school and even during your leisure activities when you sleep well. To this end, you need to deal effectively with any sleep-related disorder that you may be dealing with. Sleep disorders come in many forms, and each affects people differently, so you can expect to have a different experience from another person suffering from the same disorder. It is good to get an early diagnosis with regard to the type of problem you may be having. Diagnosing a sleep disorder happens through the presented symptoms. Some disorders, however, may need the observation of another party for effective diagnosis. Each sleeping disorder affects sleep in different ways. While some such as insomnia and RLS affect your ability to fall asleep or maintain the sleep state, others like sleep apnea affect the brain’s ability to go into deep sleep. For apnea and such similar disorders, the brain is in partial sleep, thereby limiting its ability to get into the deep sleep phase which is crucial for processes such as consolidation. Since the diagnosis of sleep disorders is not laboratory-based, you need to be alert to the signs that point to your body not getting enough sleep. If you notice some of the following signs of sleep deprivation, you need to get help to prevent the lack of adequate rest disrupting your life.
- Difficulty in falling asleep at night
If each time you get to bed you take a long time before falling asleep, then you may be having a sleep disorder. Insomnia is one such disorder where you lay awake for long periods without any sign of falling asleep. Sometimes you may fall asleep but wake up in the middle of the night and face the same difficulty of falling asleep. With RLS, you may be unable to fall asleep because of the unsettling sensation in your legs that makes you want to move your legs. This overwhelming sensation is sure to keep you up for a long time after going to bed.
- Waking up to the feeling that you are not well rested
When you are not getting adequate sleep, you will wake up not well rested. You are supposed to wake up refreshed each morning. If you do not feel restored, then your quality of sleep is not good. After a few nights of getting a few hours of sleep, you can be sure that you will not be feeling great. The brain requires getting into phases of deep rest in order to refresh. Sleep disorders prevent you from getting this deep rest. The few hours of sleep that insomnia, RLS, and other sleep disorders allow will only leave you feeling like you have cobwebs in the head.
- Daytime sleepiness
When you do not sleep at night, you can be sure that your body will want to catch up with its sleep during the daytime. You will thus find yourself dozing at the most inopportune moments. The irony of these sleep disorders is that once night comes, you are still not able to sleep. RLS happens during a position of rest, so you will struggle with sleep when you are busy with other things. When you notice increased daytime fatigue, you should check on how well you are sleeping at night. Make sure you time how many hours of sleep you are getting each night.
- Feeling lethargic
Sleep allows your body to rest in order for it to replenish its energy. When you are not sleeping well, you will suffer from low energy. You will feel lethargic and unable to catch up with your activities. Sleep disorders are draining as they hinder your cells from reenergizing. You will thus start the day low and may require energy drinks and a lot of coffee in order to make it through the day. Relying on coffee and other energy drinks also disrupt your ability to sleep, thus making the condition worse. A few days of this and you will see your sleep patterns become less and less normal.
- Mood and behavior changes
You will notice that children become cranky when they do not get adequate rest. The same applies to you. You will see changes in your behavior and moods, and in the worse way possible. You are irritable all the time and the slightest things can set you off. You are also very aggressive, which can see you getting into trouble all the time. You will work on impulse most of the time as your brain has limited ability to think clearly. When you notice mood and behavior changes, you need to check your sleep patterns as they indicate whether you have a sleeping disorder or not.
- Lack of concentration
Lack of sleep impairs your concentration level. Your brain carries out complex processes and most of these happen when you are asleep. When you are not sleeping as well as you should, these processes do not take place and thus you will have impaired brain function. You will find it hard to focus on the activities at hand. You will also find that you forget things and are absent-minded half the time. Sleep disorders are not good for your brain and will affect you in major ways. You can imagine how unproductive you will be when your brain does not work as it should.
- Low performance at work or school
The mind contributes a lot to your abilities at work and even at school. When you sleep, your brain works to consolidate what you have learned during the day. This ability allows you to learn new skills and things. When you do not sleep well, you will notice poor performance at work and at school. Poor performance and unproductivity are linked to lack of concentration, impaired ability to think and poor memory. Sleep disorders will, therefore, affect your life in different ways, and it is usually not for the best. When they disrupt your ability to sleep, you can be sure that you will see a major difference in your work.
- Troubled relationships
Lack of sleep impairs your relationships, both professional and personal. The mood and behavior changes are sure to place a wedge between you and people with whom you interact. Irritability, aggressive behavior and anger are not good ingredients for creating great relationships. Lack of sleep impairs the ability to read emotions right, thus making it hard to read the emotions others present. You will therefore not react according to the presented emotions, which may make you seem insensitive to others. This would not be good for any healthy relationship. Try to see if getting good sleep will improve the quality of the relationships that you have.
- More accident proneness
Accidents in the workplace are bound to happen more when you are not getting enough rest. Impaired brain function will affect how you handle tasks that require machine operation. The accidents can arise from the poor ability to concentrate. They can also stem from an impaired ability to carry out tasks due to slow reflexes, and poor ability to use the skills required to operate complex machinery. You can even cause accidents when you doze off while in the middle of the task. Sleep disorders, therefore, place you at risk, especially where you need full alertness to operate machines. Driving also becomes hard with chances of causing yourself and others serious injuries or worse, death.
- Depression
Sleep disorders can really contribute to increased stress and depression. The lack of sleep disrupts your mind, therefore contributing a lot to your emotional state. You will feel more despondent as you struggle with your lack of sleep. Combine that with mood swings and you will have a recipe for a depressing time. Better sleeping patterns allow for more emotional stability and help to reduce anxiety levels as well. If you notice changes in your emotional state, you need to seek help, especially when you are not getting enough sleep. It is important to know that sleep disorders affect each person in a different way. However, by knowing the signs to look for that point to the presence of such disorders, you have a chance of getting a diagnosis that will help you get the right treatment. Some sleep disorders such as RLS and sleep apnea have specific symptoms, which make it easy to diagnose. With RLS, you will feel the overwhelming sensation on your legs which some describe as burning, while others feel an itch. Sleep apnea interferes with your breathing, thus leading to respiratory difficulties, which are easy to diagnose. Keeping a log of the difficulties that you are facing during your bedtimes enables your doctor to give you the right diagnosis. If you notice any changes with your sleeping patterns, then you should start working on finding a solution. The good news is that it is possible to find solutions for your sleeping problems. Knowing what you can do is the first step of finding the solution that will work for you. The following tips will help you to enjoy better sleep, especially if you are suffering from any sleeping disorder. You will end up getting a good night’s sleep that will, in turn, translate to a better quality of life. Remember the best amount of sleep recommended is between 7 to 8 hours. This comes with a guarantee that you will feel rested and more energized the following morning.
- Seek professional help
When you suspect that you have a sleep disorder, you should seek the services of your doctor. Getting your condition evaluated ensures that you get a correct diagnosis. You may think you have a sleep disorder when all you have is a temporary condition. On the other hand, you could also be having a sleep disorder but you are not aware of it. Seeking professional help allows you to know what the problem is. A lot happens in the creation of a sleep disorder. A professional will help you determine the source of the sleep disorder. For example, RLS can be due to a number of reasons, which classify under primary or secondary factors. A professional will help you find out the right reason and give you a line of treatment that is effective to deal with your condition. By working with a professional, it means that you will not be basing your treatment on guesswork. You will have someone to monitor your progress and adjust your treatment if necessary. You can find a sleep clinic that deals specifically with sleep disorders. Your choice of clinic is vital as it will dictate the experience that you will have. The best clinic is one that has experts who are knowledgeable about your type of problem. Such will have an understanding of your symptoms and know what each point too. The best clinic will also have the ability to carry out a diagnosis. The experts will know the right tests to administer that will point out the problem effectively. Moreover, the best clinic will provide solutions that will work. You will see the difference in your sleeping patterns with the treatment they give. Even if you suffer from a chronic condition, you should be able to manage it better with the treatment you get.
- Make time for adequate sleep
Sleeping problems may arise because you are not creating enough time for sleep. You could be having so much on your daily schedule that you do not have time for adequate rest. Rising early and going to bed late gives you little time for sleeping. With time, even your body gets used to this schedule and getting it to sleep during normal hours becomes a problem. Even if you are a busy professional or student, being smart about how you work will see you place quality over quantity. The brain needs rest in order to give you better performance. By not sleeping for the right number of hours, you will counter your efforts no matter how many hours you put into work. You should plan your schedule well in order to do a lot within a given period, but still be more productive than when you put in many hours. Planning your day should see you prioritize your activities. You should tackle what you need to do for the day and schedule other matters for a later date. Even if you are working on a deadline, it is possible to produce your work within this deadline and do a good job while at it, and still get enough sleep. You should begin your day with a clear plan of what you need to do and start from there. While scheduling your day, timing is important. You should work out how much time you need to carry out a certain task and place it in your schedule. As you schedule your time, you should give sleep the required 7 to 8 hours. Therefore, as you plan when you need to be up and ready to leave for the office, you should set aside seven to eight hours before to cover the time your body needs to replenish. Habits such as procrastination and taking longer than is necessary to complete tasks cause the unnecessary delays that can eat up the time you have to get rest.
- Develop a sleep routine that you will stick to
The body will adjust itself to the routine that you expose it to. If you have a poor sleep routine, then you can be sure that your body is already used to it by now. However, with commitment, it is possible to develop a routine that is healthy for your body. You will better manage sleep disorders when you are able to make changes to counter them. For example, RLS happens when you lie on your bed for long periods. You can counter this by only going to bed when you feel sleepy enough to do so. If you get to bed and start watching a video, you can be sure that you are stimulating your brain to be active and not go to sleep. Lying for long in that restful state will trigger the restlessness in your legs and you will now have a real reason for not getting any sleep. The best routine is one that prepares your body for sleep. You should, therefore, concentrate on things that make it easy for you to fall asleep. Taking fluids before bedtime may see you have to wake up in the middle of the night to relieve yourself. You should, therefore, ensure that you do not take fluids just before you go to bed. Taking coffee and other energy drinks in the late hours will also hinder your ability to sleep. Having a sleep routine allows your body to know that it is time to sleep. When you follow this routine diligently, you will have an easier time falling asleep. If you are not sure of where you are going wrong with your sleep routine, you can discuss your current routine with your doctor. The expert will also help you to come up with a more effective routine that is best for you.
- Create the best environment conducive to good sleep
A well-lit room with loud noise in the background will not help you sleep. You might just fall asleep, but your brain will not be getting the required rest. It will be processing the noise happening in the background. You can try this by falling asleep with the radio on. You will most likely have dreams that incorporate the music you are hearing in your sleep. This will affect the quality of sleep that you are getting. The ideal sleeping environment is quiet and dark. Even if you are afraid of the dark, you can use soft low lights to provide the darkened space you need to sleep. Go for a room that is away from a noisy street or neighborhood. If you do not have the luxury of choice, be sure to incorporate noise-muting methods such as having quality windows that block out the street noise. You can also use heavy drapes that block out the noise and light coming into the room. Apart from the drapes, you should choose a quality bed and mattress that will provide a comfortable sleeping surface. A comfortable mattress will not cause any discomfort that will disrupt your sleep or make it hard for you to sleep. A creaky and unsteady bed will affect your quality of sleep. You will find that the right sleeping environment will entice you to fall asleep. You can be sure that sinking into comfortable bedding after a long day on your feet will have you sleeping away in no time. It will encourage your body to shut down even if you suffer from severe insomnia.
- Use other alternative ways to fight the lack of sleep
Even as you get treatment for your sleeping disorder, you can still use other alternative methods to manage the sleeping disorder. You can, for example, find out about the methods that people used long ago before the onset of modern medicine. Some of the methods are effective and a great substitute, especially when you are not enthusiastic about taking medication for prolonged periods. Breathing exercises that allow you to relax and therefore fall asleep are helpful. You can also use calming recordings to lull you to sleep. You can find out more about other alternatives that you can use through online resources. Your doctor may also have an option you can use as well. You may term some methods of managing sleep disorders as sketchy, but trying them might just work for you. In conclusion, sleep disorders deprive patients of their sleep, which is not a good thing for their health. Sleeping is important for vital body processes to take place. When deprived of this sleep due to sleep disorders, the body fails to function as it should. There is a risk of impaired brain activities, thus increasing the chances of decreased cognition, concentration and productivity. You will suffer decreased performance as well. In addition, you face higher risks of obesity and decreased the ability to lose weight. Moreover, changes in behavior and moods affect professional and social relationships. You will also be at risk of developing illnesses such as heart diseases and having an ineffective digestive system. With such extensive effects of these sleep disorders, dealing with them is essential. The best way to deal with the sleep disorders is to get a professional diagnosis. With so many different types of sleep disorders, the input of a professional is important to get a solution. You will get an accurate identification of the problem that you have. From there, it becomes easier to get an effective solution.You also need to do a few things that will help you manage the conditions effectively. Scheduling the right amount of time to sleep allows you to lead a more productive life even with a busy schedule. Developing a bedtime routine that encourages sleep is another way to manage the sleep deprivation as well. Lastly, you should create the ideal sleeping environment that will see you fall asleep more easily.While sleep disorders can cause issues in your life, taking a proactive approach towards managing them allows you to get a better handle on the situation. You will thus not have to deal with the severe effects of the condition that you are facing.
Getting adequate rest is critical for your body to heal and rejuvenate, and sleep is the ideal time for this restoration. Yet, daytime tiredness doesn’t necessarily mean you’re not sleeping enough. Sometimes, external factors can … Read more
Getting adequate rest is critical for your body to heal and rejuvenate, and sleep is the ideal time for this restoration. Yet, daytime tiredness doesn’t necessarily mean you’re not sleeping enough. Sometimes, external factors can disrupt your ability to enjoy a peaceful sleep. If you find yourself facing these issues frequently, it’s a good idea to see a doctor to look for potential remedies. Sleep is vital for everyone, hence its fundamental role in our daily lives. This is why many struggle to go through day and night without sufficient rest. For instance, security companies usually divide their staff into shifts, assigning some to work during the day and some at night. It’s also important to note that people have different sleep cycles, so one should not assume that everyone sleeps at night. For our round-the-clock society to function, it’s essential that its members get enough rest. The specific amount of sleep needed varies among individuals, depending on a variety of factors.
The human body has an internal clock. You should, therefore, have a constant schedule in order to keep your body in tune. Your daily schedule is influenced by what you do during the day. The daily schedule of a student and a factory worker are very different because of the nature of what they do. Your daily activities also influence the amount of sleep that you will need. According to scientific studies, adults require at least 7-8 hours of sleep per night. Many people often wonder whether having naps during the day is part of the seven hours. However, the major concern today is that many people don’t know the value of good quality sleep to their bodies. Most people are spending a lot of time working hard and smart. What they forget is that they need to be in good health in order to enjoy the fruits of their labor. Below are some of the reasons why you need enough good quality sleep;
- The best part about night time is having good sleep. Good sleep plays a big role in building the memory. The human mind does not only receive and process information, but it also stores content and reproduces it when needed. Scientists believe and have proven that sleep improves your memory. Whenever you sleep, you relax your mind. As the relaxation happens, your mind gets to store all the information that you have acquired during the day. So when you wake up, you will remember everything that happened better. This means that sleep helps your mind to wake up more refreshed and ready to acquire more information. If this continues on a regular basis, then you will be improving your muscle memory. Some couples always get into fights and disagreements because one spouse doesn’t remember their anniversary or even birthday dates. Good sleep can help with this. The other thing you should remember is that after good quality sleep, you wake up feeling better and thinking straight. When you have had a long day, you can always sleep and come up with better solutions to a problem the next day. It is believed that when you wake up, your mind has a fresh start and that is why you will have a new concept and new approach towards a problem. This is one way of enhancing creativity.
- The dream of everyone is to live a long and fruitful life. No one wants to face the bitter truth that they won’t live forever. This is the reason why most people are struggling to look young forever. In most cases, people believe that when you are young, you still have many more years to live. This might be one reason why cosmetic surgery is growing in demand. However, what many people forget is that for you to achieve a healthy lifestyle, you need proper sleep. It wouldn’t be of benefit to have all the money in the world, yet you are sick. A good night’s sleep promotes a healthy life. A healthy life will earn you more years on earth. That is one secret on how you can live long.
- The human body is created in a way that it has to rest for a while before it can continue working. However, some people deprive their bodies of the right to enough sleep. When this happens, then there will be a hitch in your daily activities. If by any chance you are a student, how do you expect to concentrate in class yet you didn’t get enough sleep? You need the sleep so that you can be able to pay attention in class. On the other hand, if you work in a factory, you need to focus on what you do so that there is better productivity for your clients. You need proper sleep to enable you to focus and pay attention to your clients’ demands; especially if you work on the policy that the customer is always right. When you have better focus in business you will definitely increase productivity. This will, in turn, earn your business more clients, which translates to increased revenue for your business. This means that sleep is at the backbone of how well you focus and pay attention to various issues in your life.
- Everybody’s life is different and unique in its own way. Life differs in the types of challenges that everybody goes through. The decisions you make determine the results of each situation you go through in life. However, some life challenges can bring about stress, especially when they are challenges that you have never faced before or those that are beyond your control. Stress has its own negative impact on your daily routine and concentration. Sleep will always relax your body and soul. This will reduce all the anxiety issues that you might have. A good night’s sleep will reduce your heart rate, which means that it will reduce your blood pressure during times when you are stressed out. Stress has been known to be one of the reasons why many people develop high blood pressure. With enough sleep, your mind and body will relax and you will wake up feeling better.
- Whenever an individual doesn’t have proper sleep, they might be sleepy during the day. This will obviously impair their vision or judgment. Sometimes you might not have enough sleep due to acute insomnia or even chronic insomnia. It is your responsibility to visit your doctor and get to the root of your problem. Can you imagine driving while you are struggling to keep your eyes open? It can be a dangerous situation because you might cause an accident. The accident you cause might claim the life of someone you love. All this can be avoided if you get the required amount of sleep. With proper sleep, you get the required concentration even when driving. Concentration and alertness is something you need in your daily activities. So always ensure that you have proper rest while you sleep.
- If you are an athlete, you will understand the importance of proper sleep before your actual game. Some games require a lot of accuracies as you play. For instance, if you are a basketball player, you need to have proper rest before a big game so that you can shoot better. Sometimes training for it can be very intense. For you to have the required speed during a game, you need to have proper relaxation. Sleep plays a big role because it helps your body muscles to relax. After the ample relaxation period, you will have all the attributes of a good player. You will have accuracy when passing the ball and you will also have good reaction time during the game. When all players in a team have these qualities, then the team will stand a better chance of winning. If you are a professional weightlifter, you understand the importance of having proper sleep. A good night sleep will ensure that your muscles heal properly after training. When you train at the gym, your body gets tired and your muscles wear out. On the other hand, when you have enough sleep, your body tissues get enough time to heal and this results in stronger and bigger muscles.
- The immune system in the human body helps to keep the body healthy. When your body is free from any illness, then it means that you are healthy. You can boost your body’s immunity by eating several types of foods. In addition, sleep has also been proven to boost your immune system. When you go to sleep, your body produces protective proteins which liaise with the white blood cells to fight any infection. Some diseases like the common cold can be moderated with a strong immune system. Have a healthy life by boosting the functionality of your immune system.
- In the current generation, people are finding it easier to communicate because the whole world has been turned into a global village through the availability of the internet. People can communicate through social media platforms. This might not be the case when you have to wake up and go to work. At your workplace, you will need proper communication skills that will enable you to interact with your colleagues. This might be a challenge if you didn’t have enough sleep. When you are sleep-deprived, you will feel tired and sometimes you might become moody. This will, in turn, have an effect on your emotions. When you have emotional challenges, it gets hard to socially interact with others. To be on the safe side, always ensure that you give your body the required amount of good quality sleep.
- Sleep has proven to play a big role in a couple’s sexual life. Less sleep can reduce the levels of your testosterone. This will, in turn, reduce your libido. When you have a lower libido, then you will not be able to function as required during sex. Lower testosterone will also reduce your sexual interests. If you suffer from chronic insomnia, you might develop erectile dysfunction. In women, lack of sleep will result in sexual distress. This is a condition where the lady has zero interest in sex. This can result in a problem in the relationship, especially if the man has a higher libido. To be on the safe side, everybody should have enough sleep. Enough sleep has more benefits to the body than less sleep. If you have challenges sleeping, then you need to visit the doctor and seek medical guidance.
Wonderful things you should always know about sleeping hygiene
Sleeping hygiene basically includes practices that each individual takes part in before going to bed. These are tips that have been proven to be effective by most individuals. However, sleeping rituals differ depending on the individual. These rituals help to influence your sleep cycle. They will play a role in what time you sleep and wake up. The same sleeping rituals will play a role in how the following day will be like. This is because how you tackle the next day largely depends on how well you sleep the previous night. Sleep has proven to have many benefits for both your health and well-being. There are two major types of sleeping hygiene. These are; good sleeping hygiene and bad sleeping hygiene. Good sleeping hygiene is the good practices you do before you sleep whereas bad sleeping hygiene is the bad practices that will result in you not having high-quality or enough sleep.
How then do you maintain a good sleeping hygiene?
- Everybody spends his or her day differently. This means that everyone knows how much sleep they need so they can function well. The amount of sleep a young child needs is different from the amount of sleep an adult needs. Similarly, the amount of sleep you need when on holiday is different from the amount of sleep you need when you are working. As an individual, you need to assess your condition and decide on the minimum amount of sleep that you need. This will help you establish a good sleep routine.
- For you to achieve a good sleep routine, you need to determine what time you sleep and wake up. You need to instill a certain kind of discipline into your body. A sleeping pattern can only be achieved if you train your body to be going to bed and to be waking up at specific times. Sleeping routines change depending on the occasion or the occupation one is in.
- You need to train your body to sleep in less bright light. You might go to bed at your normal bedtime but find it difficult to fall asleep because there is too much bright light. Bright light will stimulate your eye muscles, which will make it hard for your mind to shut down and sleep.
- The current millennium has a lot of communication gadgets. These gadgets are available to help make communication better. However, because of the light that their screens emit, they make it very difficult to fall asleep. Therefore, in order to have an easier time falling asleep, keep your gadgets away half an hour before going to bed. This is so that you have time to decompress and relax.
- Caffeine can be found in products like tea and coffee. When you take hot tea before you sleep, you will likely not be able to go to sleep, and this can mess with your sleep cycle. You should, therefore, try to avoid anything that has caffeine half an hour before going to bed. Dark chocolate made from cocoa has caffeine too. Caffeine plays a big role in stimulating your body, and this will mean that you stay up longer struggling to get sleep.
- Exercise will help you maintain a good sleeping hygiene. This is because some exercises will help you to reduce your stress levels. However, you need to ensure that you don’t indulge in strong and vigorous exercises. Vigorous exercises before bedtime will make it hard for you to sleep in good time. You can always have these during the day. One hour before bed, you can have light exercises such as yoga that will cool off your body and send you to sleep.
- You need to ensure that you have dinner early enough. When you do this, you give the body ample time to digest the meal. If you eat and immediately head to bed, your body will focus on digestion, and this might cause a lot of discomfort during sleep. Discomfort is one reason that leads to sleeping disorders. If you want a steady sleeping pattern, then you should always make sure that you have your dinner prepared and eaten in time.
The undeniable bedtime rituals that will lure you into a good night sleep
In life, everyone has those few traditional practices that they do to ease them to sleep. The day you forget doing this practices, you might end up finding it very difficult to sleep. In most cases, these practices are also part of good sleep hygiene. These rituals relax your body and shut down your brain as you prepare to sleep.
Below are the most used rituals that have proven to work;
- The best thing about the current millennium is technology. Through technology, a lot has improved. The internet has become one of the most common things around the world. Technological advancement has also led to the invention of better electronic gadgets. However, some of these gadgets are to be blamed for people having poor sleeping patterns. You should, therefore, ensure that you always switch off any form of technology before bedtime. You can do this an hour beforehand. This will help your brain to shut down slowly and eventually you will be able to sleep once you get to bed. In most homes, switching off wifi or any form of internet connection helps in preparing for bed. You should also ensure that no electronic gadget is running.
- The best thing about reading is that you get to acquire more knowledge. This is a habit that you should practice before you sleep. The reason why reading is recommended at this time is that your eyes will have to focus on the small words on the page. Your eyes will also be expected to move from one line to another. With time, the eye muscles will get tired and you will feel exhausted since your brain will also be relaxed. The eye muscles can’t focus for that long. Therefore, make sure you always keep a book on your nightstand.
- Your body has mechanisms that ensure the right temperature is maintained. It does so to ensure that external temperatures don’t affect the body functions. If the external environment is too hot, then with time you will start sweating and before you know it, you will be up. If the room is located in an extremely cold area, then your body will need more warmth to ensure you get the required sleep. In order to sleep immediately you get to bed, you need to adjust your air conditioner to room temperature an hour or two before bedtime. This way, you will have the required sleep all night long until the alarm wakes you up.
- You might be wondering whether taking milk is really important before going to sleep. Some people just have milk in the morning because milk has almost all the food components that your body needs. However, milk has tryptophan that plays a very big role in the relaxation and calming of the body. When your body is calm and relaxed, you can sleep peacefully.
- The reason why you need a warm bath before you sleep is that a warm bath plays a big role in relaxing your body. If by any chance you had a long day and you are tired, a warm bath will help calm your aching muscles before you sleep. You can make it a habit and see how it will work wonders for you. You will be able to sleep without any worries.
- The best thing about getting a light massage before bedtime is that it lowers any form of anxiety. Anxiety has proven to be one reason why most people experience insomnia. When you kick out anxiety through a light massage, then you will restore your wonderful sleeping routine. On the other hand, massages also reduce body pains which in turn stimulate relaxation within the body. If you have no pain, you can concentrate on sleeping peacefully. However, you should avoid any form of deep tissue massage before you get to bed. This is because it might cause some pain and thus make it hard for you to sleep.
- Meditation is one way that can actually help you sleep properly. This is because meditation plays a very big role in calming your body. During meditation, you are advised to concentrate on your breathing. When you get your breathing to become regular, you also relax your mind and body. The same case applies to yoga and stretching. You can actually do light yoga stretches before you sleep. The reason why yoga is preferred by many is that it is one way of releasing stress. Once you have no stress, then it gets pretty easy for you to sleep.
- Your eyes and brain require darkness or dim lighting to activate sleep immediately after you go to bed. How do you achieve this? The light from your television set or even laptop can keep you awake for long because it gives the illusion of daytime. The best thing, therefore, is to ensure that you don’t expose your eyes to any form of bright light when going to sleep. Switch off all the lights half an hour before bedtime. If you really need some light, invest in some dim lights.
Terrible rituals you should never do before getting into bed
Rituals are majorly practices people indulge in before doing something important. Bad sleeping rituals are common mistakes people make that actually alter their sleeping schedule. These are the things you should never do before going to bed;
- The reality about life is that you might sometimes be on medication. The medication should always be approved by your doctor. However, you need to have a discussion with your doctor about the effects that the medication has on you. Some drugs can make it easy for you to sleep. However, if the pills will in one way or another alter your sleeping pattern, then it will be better if you take them early before bedtime. If you are an athlete who uses supplements, you should also inquire more about how they affect your sleeping pattern. You need to know whether they will cause any problems during sleep. This way, you will be able to arrange on when and how to take them.
- By now, you probably know that the body requires adequate water to function. However, you shouldn’t drink too much water at night right before bed. The reality is that water plays a very big role in digestion. However, if you drink too much water before bedtime, your body will focus on the absorption of the water and you will end up breaking your sleep from time to time in order to go to the bathroom. This will affect the amount and quality of sleep that you get. Sometimes it gets hard to fall asleep after you have woken up.
- Most people think that making calls takes a lot of time and that it can actually stop you from sleeping. However, texting is now the new habit that can make you stay up all night and before you know it, it’s morning. This is because the current mode of texting allows participants to share audios and videos. This way, messaging becomes very interactive and interesting. This will not help to build brainpower. Instead, it will give you difficulties sleeping once you are done because your brain is active. So, keep your phone away before bedtime.
- Working out is healthy for the body. That is why it requires a specific duration of time just like any other activity you do during the day. However, you should avoid having intense workout sessions before going to bed. When you work out, your whole body becomes stimulated and will take a longer period to cool off. This means that you will have to wait for some few hours before you can actually get to sleep. This will automatically affect the amount of sleep you get in a night. However, you can indulge your body in simple exercises like stretching and yoga just to calm the body down before you sleep.
- Tea and coffee are all stimulants. Any stimulant will activate your senses. You need your body to be calm and relaxed during bedtime so as to sleep well. You should avoid having beverages like tea or even coffee at that time. Some products that have caffeine, like chocolates should also be avoided before going to bed. Dark chocolate made from the cocoa plant contains caffeine that will stimulate your brain system instead of shutting it down.
- Working from home has become a common habit with a lot of people, especially when they have a deadline to beat. It gets extremely stressful for them and such issues can cause acute insomnia. The best thing you can do for yourself ensures that you avoid opening your work emails before going to sleep. This way, you can ensure that you don’t walk into bad work surprises. You will be able to have proper sleep without any panic or nervousness.
- It is very bad for any couple to pick a fight before going to bed. You should always ensure that you go to bed as a couple when you are relaxed and happy. In most cases, the fights always lead to stress, and stress will often lead to insomnia. To be on the safe side, you should avoid any form of wrangles with your loved ones before getting into bed.
- You should avoid alcohol before getting into bed. Alcohol plays a major role in causing sleep disorders. In most cases, alcohol will mess around with the brain receptors. This means that your brain will find it very hard decompressing and shutting down. Eventually, you will have difficulties falling asleep. Smoking, on the other hand, contains substances that will also stimulate your brain receptors. Your brain receptors need to cool off, and the brain can’t cool off when it’s being stimulated. Therefore, avoid any alcohol and smoking before bed. This way, you will be able to enjoy a good night’s sleep.
If you ever catch yourself behind the wheel while feeling sleepy, understand that you’re not alone in this experience. Sadly, driving while fatigued is a major problem in the U.S., with studies showing that around … Read more
If you ever catch yourself behind the wheel while feeling sleepy, understand that you’re not alone in this experience. Sadly, driving while fatigued is a major problem in the U.S., with studies showing that around 60% of people have driven in such a state at least once, and about a third have even dozed off at the wheel. Though it might seem harmless to drive while tired, the consequences can be severe. Falling asleep can happen without warning, raising the risk of an accident that could injure both the driver and others. Learn more about the dangers of drowsy driving.
It is important to know that sleep deprivation has similar effects on your body as drinking alcohol. For example, when it comes to drowsy driving vs. drunk driving, being awake for 18 hours will make you drive like you have a BAC of 0.05%. To be clear, by law, 0.08% is considered drunk. If you haven’t slept for 24 hours, it’s like you have a BAC of 0.10. Drowsy driving mostly occurs when a driver didn’t get enough sleep, but it can also happen due to medications, shift work or untreated sleep disorders.

What Is Drowsy Driving?
Drowsy driving is also known as driver’s fatigue, and it occurs when an individual is too tired to operate a motor vehicle. Due to this, the driver puts himself and others at risk. Some of the most common causes of drowsy driving are inadequate sleep, untreated sleeping disorders such as narcolepsy and sleep apnea, shift work, driving without making regular breaks and the use of sedatives, hypnotics and other medications that may negatively affect your alertness and induce sleepiness.
The effects of driver’s fatigue can vary from person to person, but most of them have slower reaction times and experience short-term memory loss while driving. Drivers can also sometimes drive aggressively.
Who Is at Risk for Drowsy Driving?
Every driver is at risk, but the issue is more common among certain groups.
Young Drivers
Inexperience combined with sleepiness and tendency to drive at night particularly puts at risk young males aged 16 to 25. Sleep deprivation is another crucial factor. Most adults require seven to eight hours of quality sleep per night, but young adults require at least nine in order to achieve the same levels of functionality. However, an average adult gets only between 5 to 7 hours of sleep per night.
Young adults are encouraged to develop a healthy sleep schedule and to avoid alcohol and electronics at night to reduce the risks of drowsy driving. Inadequate sleep, tobacco, alcohol consumption and using electronic devices at night are one of the leading causes of sleep deprivation among individuals aged from 16 to 25.
Shift Workers
Shift work is as any work schedule that falls outside the standard work time of 9 am to 5 pm. Shift work may include night shifts, double shifts, or rotating shifts. In most cases, shift work is done where round-the-clock personnel is needed, such as in law enforcement and healthcare.
There are ways shift workers can reduce the risks of drowsy driving. For example, ride sharing will reduce their time behind the wheel each week. Also, long or overtime shifts should be avoided if they plan on driving long miles.
Commercial Drivers
Commercial drivers typically drive high miles, and at night, and due to this, they are particularly at risk for fall-asleep crashes. In order to decrease the risk of drowsy driving, commercial drivers shouldn’t operate their vehicles between 12 am to 6 am, and 2 pm to 4 pm because these are the period when most people get sleepy. It is essential for them to take regular breaks, napping for at least 20 minutes and then allowing an extra 15 minutes to wake up. Power naps can help them a lot to restore energy, and increase their alertness.
Ride Sharing Service Providers
Although companies such as Uber and Lyft have regulations which involve their drivers to take regular breaks, they often work a second job which further increases their sleep debt.
Business Travelers
Business trips typically involve long journeys, in the case of international travels, and when you always have to adjust to the local time, it may affect your circadian rhythm and sleep cycle. The transition period or jet lag can especially be tricky and cause sleepiness.
To prevent or lower the risks of drowsy driving, business travelers should go to and from airports using car services. The effects of jet leg can also be reduced by gradually adjusting to the local time of the place you’re going to stay in. It is best to try to follow a sleep schedule that aligns with the time zone of your destination. Avoiding alcohol, smoking, and caffeinated beverages will also help to ease the effects of jet lag.
People with Untreated Sleep Disorders
Many sleep disorders can cause drowsiness. The most common sleep disorders that cause sleepiness are insomnia, sleep apnea and narcolepsy. A driver with an undiagnosed sleep disorder is at high risk of causing or being involved in a motor vehicle accident. For example, people with untreated obstructive sleep apnea are seven times more likely to fall asleep behind the wheel. Insomnia also increases fatigue.
Am I too Drowsy to Drive?
Same as drunk driving, drowsy driving makes it very hard to pay attention to the road and slows down your reaction time. Although sleep deprivation has similar effects on your brain as drinking alcohol, drowsy driving and drunk driving don’t always look the same on the road. A drunk driver may drive slowly and try to react, while a sleepy driver can nod off while still going very fast. Since sleep deprivation significantly slows down your reaction time, drowsy drivers won’t always break when something happens right in front of them.
The best way to prevent drowsy driving is to learn to recognize its signs. If you believe your fatigue level may be impacting your driving, here are some of the warning signs of drowsy driving you should look out for, no matter whether you are the driver or a passenger.
- Inability to focus
- Constantly yawning
- Heavy eyelids
- Bobbing your head
- Drifting from your lane
- Missing signs and turns
If you notice such behavior, it is vital to safely pull over the car and take a 20-minute nap. Also, buy a cup of coffee to stay more alert. If there is another driver in the car, let him or her to drive instead of you. If you are driving long miles, you should drive during your most alert period of the day and take regular breaks. These precautions seem simple, but they can help a lot to lower the risk of falling asleep behind the wheel and causing a drowsy driving accident.
Ways to Keep Yourself Up While Driving – Drowsy Driving Prevention
The best ways to prevent drowsy driving is to get some sleep. Before driving long miles, you have to get enough sleep and take breaks every few hours to rest. By learning to recognize signs of drowsiness and fatigue, you could avoid driving sleep deprived.
Avoid Driving
If you know your circadian rhythm is generally unstable or naturally drowsy, you have to avoid operating a vehicle, especially if you plan to drive for long miles.
Caffeinate Wisely
Never forget that coffee and other caffeinated beverages are not a replacement for sleep! Coffee and energy drinks can temporarily help you stay alert and improve your focus, but keep in mind that these effects last only for 30 minutes, and also require around half an hour to kick in.
Sleep Tight
Before going on a long road, get a good night’s sleep! This is the best way to ensure you won’t feel tired or drowsy on the road.
Drive Together
In most cases, drowsy driving accidents are caused by drivers who were driving alone. Therefore, if you are going on a long trip, bring a friend with you. A recent UCLA study found that bringing a friend can significantly decrease your chances of falling asleep at the wheel. Also, if your passenger has a license, he can replace you once you become sleepy.
Take a Break
When you need to get a nap, use a rest stop. A rest stop is a safe space to park your car and take a nap, grab a bite, and similar. Consuming a caffeinated beverage may also help you to stay alert. However, you should keep in mind that coffee and energy drinks will make you feel refreshed only for 15 to 20 minutes. Never forget that caffeine is not a replacement for sleep.
Check Your Meds
If you take medications regularly, it’s important to read the warning labels and see if they might affect your alertness or cause sleepiness. Medicines don’t have to be particularly prescribed for sleep disorders in order to induce drowsiness. Medication types such as narcotic pain relief pills, antidepressants, tranquilizers, antihistamines, and muscle relaxants can trigger sleepiness.
Bring in Some Fresh Air
Being in stuffy car interiors can easily make us sleepy. So, getting plenty of fresh air can also help to increase your alertness. Make sure to occasionally open the car windows or adjust the vent controls to bring in some fresh air.
Listen to Music
Listen to music, especially if you are driving alone. Rather than listening to loud music, we recommend listening to energetic music. This is also one of the way to prevent falling asleep while driving.
Drive with the Sun
Whenever possible, drive during the day, or even better, when the sun rises. Sun will stimulate melatonin production and your circadian rhythm, keeping you more awake and alert during the day. Sunlight stimulates your brain and will also extend your reaction time while at the wheel. Lastly, natural sunlight is an excellent source of vitamin D, which can help you sleep better at night.
Is Driving While Drowsy Illegal?
Driver’s fatigue can put you in jail. In most states, there isn’t a law that specifically relates to drowsy driving, but it’s mostly considered as a form of reckless driving, similar as driving under the influence of alcohol or drugs.
By acting as a responsible driver and educating yourself about the risks and warning signs of drowsy driving, you will avoid being a part of the 328,000 drowsy driving accidents that occur every year. The NHTSA and the CDC estimate that 109,000 of those crashes results in injuries, while 6,400 result in death. Also, don’t forget that we mentioned sleep-deprived driving is very similar to driving under the influence. Being awake for 24 hours straight is equal to a BAC of 0.10%, and that significantly higher that the legal limit of 0.08% in all US states.
The vast majority of us loathe the idea of waking up in the morning. The mere fact that it’s early and the air is crisp gives us every excuse to hit the snooze button for … Read more
The vast majority of us loathe the idea of waking up in the morning. The mere fact that it’s early and the air is crisp gives us every excuse to hit the snooze button for “just another five minutes.” For a lot of people, there’s no greater pastime than sleeping in, especially enjoying a leisurely nap on a slow weekend afternoon. Sadly, this pleasure is something only a handful of adults can afford nowadays. Leading scientific institutions along with the American Sleep Association have discovered that about 70 million adults in the U.S. struggle with initiating and maintaining sleep. Some even dread the thought of going to bed at night due to the discomfort they experience while trying to sleep. These individuals often delay bedtime until they’re completely worn out.
That brings many questions to our minds –
- What causes the distressing symptoms during sleep?
- Are most sleep disorders hereditary?
- Is it possible to treat and cure sleeping disorders?
- What kinds of discomfort qualify as sleeping disorders?
- What do medicine and sleep science call these disorders?
- What are the dangers of experiencing these?
- Who do sleep-related disorders affect?
What are the typical signs of parasomnia?
Sleeping disorders can be of various types. Almost all children experience nightmares from time to time. You may remember a couple of the unpleasant dreams you may have suffered as a child. Common recurring themes of nightmares among adults include public nudity, teeth falling out and running but not being able to move. According to sleep experts and psychologists, these nightmares are unpleasant but quite common. They do not qualify as sleep disorders unless they are causing you to wake up with physical discomfort in the middle of the night or keeping you awake for long hours. In most cases, we experience unusual dreams, but we remain asleep throughout the process. They do not cause us to frail about in our bed, strike out or to sit up and scream in a delirium. When these symptoms come in the picture, the case quickly escalates to sleeping disorders of the class parasomnia.
There are a few classic symptoms of parasomnia include the following –
- Abnormal movements
- Emotions
- Strange perceptions
- Overall unusual behavior
- Acting out dreams or nightmare while falling asleep or during sleep
Researchers define parasomnias as dissociated sleep states that lead to partial arousals. They associate these stages with transitions between REM or NREM sleep and wakefulness. Interestingly, sleep disorders do not always stem from nightmares or unpleasant dreams. Although a bizarre and scary dream may affect a person more, he or she is equally likely to act out the mundane dreams as well. It is common for children to do so, but when adults start enacting dreams of sexual nature in their sleep, it can be particularly embarrassing and scandalizing.
What are the two basic types of parasomnias?
Considering the fact that over 10% Americans currently suffer from one kind of parasomnia or another, there must be several studies that can shed some light on the cause, treatment and potential cure of the disorder. Before we go into that, we should try and understand the classification of these sleep disorders.
Non-rapid eye movement (NREM) parasomnias
The NREM parasomnias typically occur during slow-wave (stage 3 and 4 of NREM) sleep. That happens when the person is somewhere between complete sleep and wakefulness. There is physiological activation that causes the person to exit the full suspension of physiological movement, but he or she continues to sleep and dream. Research shows that these stages involve the activation of the cognitive process, the motor system and the autonomic nervous system (ANS).
Night terrors and confusional awakenings are more common during the childhood of a person than they are during adulthood. One expects these issues to go away as the child transitions into the teenage and eventually, adulthood. When the same incidents recur among adults, they likely suffer from parasomnia. Specific factors including sleep deprivation, depression, and medication for depression, physical stress and emotional stress can induce NREM parasomnias in adults.
During NREM parasomnia, a person can expect one or more of these symptoms –
- Sleep-eating
- Night terrors
- Sleepwalking
- Sleep-sex
- Grinding of teeth
- Restless legs syndrome (RLS)
- Rhythmic movement disorder
- Somniloquy (sleep-talking)
Rapid Eye Movement (REM) parasomnias
Contrary to NREM parasomnias, these happen during the REM stage of sleep. The person loses atonia or muscle paralysis during this stage, which allows him or her to move about while dreaming. While REM is ubiquitous among adults, people rarely seek counsel or treatment. Patients experience a high risk of injuries resulting from the sudden movements, and they pose a threat to the co-sleeper as well. Patients do take precautionary measures that range from barricading themselves with pillows to sleeping on a low bed or mattress.
Research shows that the telltale signs of REM sleep disorders include the following –
- The sufferer is male (90% of RBD patients are male)
- The age of onset varies between 50 years and 65 years, but anyone between 20 years and 80 years can experience RBD on and off.
- Screaming, mumbling, swearing and other vocalizations may be present.
- Usually happens during the latter half of the (REM) sleep period.
- They might have other neurodegenerative diseases like Alzheimer’s, multiple system atrophy (MSA) and Parkinson’s.
- The person might be on anti-depressants and other psychoactive drugs.
- Over 45% of the times, the sufferers have a history of alcoholism and alcohol use.
Catathrenia is a form of REM sleep disorder during which a person is likely to hold his or her breath. It involves groaning during expiration. It does not have any known associations with obstructive sleep apnea and somniloquy. The person experiencing this sleep disorder is usually unaware of the noise, but the co-sleepers might find it disturbing. Interestingly, although the sufferer is unaware of the sound, they often find themselves awake in the middle of the night after constant groaning.
Why is insomnia not a type of parasomnia?
That finally brings us to insomnia. Apart from pop songs and Hollywood, social media has made ‘insomnia’ a trend. When a person suffers from the lack of sleep for two nights in a row, the person claims himself or herself as an insomniac. What we need to understand is that it is a disease that renders a person unable to fall asleep at desired or socially acceptable bedtime. As a result, the person finds himself or herself awake till 3 am or 4 am in the morning, for multiple nights in a row. When a person suffers from the lack of sleep for over two months, then the doctors and sleep experts pronounce it as a case of insomnia.
It can be recurrent and intermittent, or it can be chronic. In cases of chronic insomnia, a person is unable to fall asleep in spite of staying awake for over 24 hours at a stretch or suffering from sleep deprivation for a couple of days. It is indeed a sleep disorder, but it is not a form of parasomnia. While parasomnia involves abnormal movements and the inability of a person to remain asleep, insomnia consists of the ability of a person to fall asleep. The leading causes of it include increasing consumption of caffeine, alcohol or wakefulness stimulating drugs. It can also be a result of depression, chronic pain, psychological stress, physical injuries, restless legs, menopause, premenstrual stress syndrome, and hyperthyroidism.
Usually, cognitive therapy, sleep therapy and sleep medication help with the treatment of insomnia. Since the person has no problem staying asleep and with the quality of rest, there is no question of rectifying behavior during sleep.
What are the different types of primary parasomnia?
We should get about 8 hours of sleep each night. Experiencing parasomnia can keep you from getting the rest you require. Here are the six most common types of parasomnia that can keep you up at night and doze during the daytime –
- REM sleep behavior disorder (RBD) – During RBD, the sleeper’s brain is in a highly active state. The EEG shows the activities to be similar to that of the waking stages. Dream-enacting is the typical sign of RBD that can affect men more frequently than women. Although the exact causes remain unknown, this recurs with neurodegenerative conditions. It can eat away 20% to 25% of the sleep period. Just like most REM sleep disorders, it is common among the elderly and middle-aged men. There are pieces of evidence to suggest that RBD may be hereditary and genetics may have a significant role to play in it.
- Sleepwalking – Sleepwalking or somnambulism is more common among children than it is among adults. When children do not outgrow the habit of walking in their sleep even during their tween and teen years, it is worrisome. Adults exhibiting sleepwalking tendencies often wander onto the streets from their home while they are sleeping. There are records of people unlocking their doors, starting their cars and driving while sleeping as well. It is very dangerous for the people and the ones involved in these incidents. However, trying to jostle someone awake is not a good idea during one of their episodes. It is better to guide them back to bed gently and to stay with them until they are back to regular sleep. Certain medications show promise in the treatment of sleepwalking. Benzodiazepines, anticholinergics, antipsychotics, and selective serotonin reuptake inhibitors are potential treatments of the condition, although there is no cure. The sufferer should avoid high beds, bunk beds and bedrooms with French windows for safety reasons. Prolonged sleep deprivation, caffeine, and alcohol worsen the disorder.
- Night terrors – Night terrors are very different from nightmares. They are common during NREM sleep, while nightmares occur during the regular dreaming (REM) phase. When a person experiences night terror, he or she is likely to struggle, sit up, scream and make gestures. It can be frightening for the co-sleeper. The person experiencing the sleep terror might even have his or her eyes open. However, they are not likely to have any memory of the incident the next morning. The person is usually in a delusional state and is not fully awake. Therefore, trying to reason with the person or coaxing him or her back to sleep does not work. It affects only about 3% of the adult population. Two episodes may have days or weeks between them. They are usually unpredictable. They may even occur multiple times during the night. Research shows a genetic dependence and autosomal mode of inheritance of the disease. There are not a lot of treatment options, but psychotherapy, counseling, benzodiazepines and tricyclic antidepressants can help in the treatment of night terrors among adults. Behavioral therapy usually works effectively for children and young adults.
- Nocturnal sleep-related eating disorder (NSRED) – NSRED is a modified form of somnambulism or sleepwalking. Those sleepwalkers, who regularly walk to the fridge or kitchen and eat while they are at it, suffer from this bizarre yet severe form of sleep disorder. It is an NREM sleep disorder just like somnambulism. It is especially dangerous when the sleepwalker indulges in food items they are allergic to. People who have diabetes, Celiac disease, and cholesterol related problems are always are a higher risk of damaging their health if they suffer from NSRED. The danger catapults when the person tries to use sharp tools in his or her sleep or tries to use the stove and microwave for cooking, while asleep. The treatments are prolonged and involve extensive counseling, like sleepwalking. There is no long-term cure, and without proper therapy, the problem can recur within a couple of days, weeks or months. There is no particular trigger, although discomfort during sleep, sleep deprivation, increased stress and alcohol consumption increase the chances of its recurrence.
- Teeth grinding – Bruxism or teeth grinding is a distinct form of parasomnia. Children often grind their teeth during sleep and parents attribute that to bad dental hygiene, caries, and even worms. Once they enter their early teenage years, the problem should go away on its own. However, there are instances when young adults and adults have preserved this habit. Apart from causing fatigue of the facial muscles, long-term bruxism can lead to attrition. Repetitive grinding of teeth can cause teeth to wear, crack and chip. Dentists commonly refer to it as a parafunctional activity. It currently affects between 8% and 31% of the population. Sleep bruxism affects the males and females in a population equally. Psychological and physiological stress equally affects the incidences of sleep bruxism among both the sexes. Further evidence from studies of affected individuals shows that a majority of the sufferers have had at least one family member, who showed signs of teeth grinding. Another research into the genetics of bruxism showed that people with teeth grinding are more likely to pass it onto their children.
- Unspecified parasomnia – When a person exhibits more than one classic symptom of different types of parasomnias, sleep experts, psychiatrists and doctors usually state that he or she has unspecified parasomnia. There are instances when an adult shows symptoms of RBD, somnambulism, somniloquy, and NSRED at the same time. That is where things become complicated. It is any way challenging to diagnose and treat any form of parasomnia, but when the disorder comes in several forms, the potential treatment becomes almost impossible. Multiple factors contribute to the sleep disorder and as a result, addressing just one issue will not help the patient. The causes vary significantly between people, but in the majority of the cases, they revolve around physiological problems. There might be problems with the area of the brain that minds the wakefulness and sleep states. He or she might suffer from hormonal imbalances.
What causes parasomnia episodes?
We have gone through the six most prominent types of parasomnias among people. These sleep disorders interfere with sleep quality and lead people to feel sleep deprived. It is only fair that the sufferers get to know what causes their fatigued sleep and sleep disturbances. However, even with the advent of medical technology, the understanding of these disorders is limited. Medical professionals, psychologists, and sleep experts are still trying to figure out the exact causes of these disorders and the triggers for individual episodes.
There have been certain theorizations and facts that point towards possible causes. Here’s a list of factors that might be keeping you from getting proper rest –
- REM and NREM disorders might have their roots in degenerative neuronal diseases. Parkinson’s, Huntington’s, Alzheimer’s, and Multiple System Atrophy (MSA) or Shy Drager syndrome can lead to parasomnia.
- Several types of parasomnia have their roots in human genetics. Bruxism, sleepwalking, sleep-talking, and RBD may have autosomal inheritance patterns. Children with any form of sleep disorders are likely to have at least one parent, who suffers from the same.
- Middle-aged and senior men are more likely to suffer from parasomnia episodes regularly.
- Preceding days of the lack of enough rest can lead to parasomnia (REM) sleep disorder episodes.
- There is significant dependence on the incidence of sleep disorders and addiction. Addiction to prescription medication, hallucinogenic drugs, alcohol, and nicotine worsen the cases of parasomnia.
- Improper sleep hygiene, uncomfortable humidity and temperature settings, allergy attacks during sleep and insufficient (mattress) support can start an episode of insomnia.
- Studies show that people, who indulge in coffee and caffeinated drinks right before bedtime have higher chances of suffering from sleep disorders.
- Eating fatty and fried food can trigger acid reflux and heartburn that can lead to cases of parasomnia among the predisposed population.
- Physical stress including discomfort due to digestive challenges, injuries, and chronic pain can trigger episodes of REM or NREM disorders.
- Previous cases of brain injury, brain tumors, tumors of the brainstem and craniotomies always increase the chances of the patient developing parasomnias in the future.
Parasomnia is a heterogeneous disease. There are several categories and subcategories. Therefore, it is only fair that there are multiple potential causes of the same, instead of just one.
What are the other causes of parasomnias?
Sometimes, the inability to get enough rest per night does not stem from heredity or physiological stress. Sometimes, disorders of other organ systems lead to disturbances in sleep quality and duration. Typically, arrhythmias, dyskinesias, convulsions, and regurgitation can lead to disturbances during sleep. Sleep apnea, allergic reactions, and breathing difficulties often keep people in a delusional stage when they are trying to fall asleep. Evidence suggests that high fevers from diseases like malaria and dengue usually keep people in such semi-awakened states. These stages of semi-wakefulness also qualify as parasomnias, but unlike RBD and sleepwalking, the causes are not in the brain.
When separate organ systems (either one or multiple) contribute to such confused states of sleep and wakefulness, researchers and doctors prefer to call it secondary parasomnia. Idiopathic or primary parasomnias are prevalent among male patients, but secondary forms of the disorder depend on the incidence of the disease that causes the disturbances of sleep. For the treatment of secondary parasomnias, cognitive behavior therapy, modulation of sleep hygiene and administration of medication to treat sleep quality are not enough. You need to think about getting treatment for the underlying disorder or disease that is causing the parasomnia. Sometimes, corticosteroids are necessary for the treatment of the same.
What are some sleeping habits that can improve your quality of nightly rest?
It is understandable that your behavior during the day will impact your nighttime rest. What you eat how much physical exercise you get and how long you spend in front of the laptop will determine the quality of sleep you get during the night. You will often come across sleep advice blogs and medical experts, who will encourage you to maintain a sleep journal. Undergoing cognitive behavioral therapy can improve the quality of sleep you get each night. It can enable you to address the thoughts and habits that keep you from getting good quality rest each night.
If you are facing difficulty in getting enough rest on a regular basis, you can try the following –
- Maintain a consistent sleeping schedule. It might be difficult in the beginning, especially if you have the habit of falling asleep multiple times per day. Wake up and leave the bed at a consistent hour, even when you feel like you need more sleep.
- Do not go to bed early in the evening, even if you are sleepy. Stick to a particular bedtime that is neither too late nor too early. Going to be between 10:30 pm and 11:00 pm should give you enough time to get proper 8-hour rest.
- Make sure your bed is the place for sleep and sex only. Do not watch TV on your bed. Do not fidget with your phone or tablet.
- Stay away from electronic devices including your television right before bedtime. Switch off your mobile phone, laptop, and TV 30 minutes before bed.
- Invest in a reliable humidifier and air conditioning system. Dust your bed regularly and use clean sheets.
- You can try using a white noise machine. Sometimes, leaving the TV switched on in the next room helps people sleep due to the constant drone it generates. Moving fans, TV and the hum of home appliances can be your “natural” source of white noise.
- Do not eat within an hour of bedtime. If possible, eat a light meal devoid of too much fat and spice. If you get hungry at night while you are lying awake, get up and eat a light snack. Keep crackers handy (but out of bed).
- Always try to work out a little in the mornings. Meditation and yoga after waking up can help you boost wakefulness during the day.
- Stay away from caffeine and caffeinated drinks in the evening. Even tea has some amount of caffeine. So be careful about what you drink.
- Avoid sugary food. This step is especially critical if you suffer from hypoglycemia or diabetes. The rise and fall in glucose levels will determine your hormone content that dictates sleep.
- Do not drink alcohol, smoke cigarettes or eat junk food right before bedtime. Do not drink too much water either.
- Do not expose yourself to high-intensity blue light in the evenings. Keep the bedroom dark, comfortable and quiet.
- If you are taking any new medication that might be interfering with your sleep quality, you might want to speak with your doctor.
These are a few ways you can improve your sleep hygiene over time. These healthy sleeping habits can enhance your ability to gain the rest your body and mind deserves each night. Always remember that there is a difference between the inability to fall asleep and lousy quality sleep. That should help you understand why you need specialized therapy and treatment, or why regular sleeping medication will not help you as much as a patient suffering from insomnia.
Do you have parasomnia?
Not sleeping well night after night, yet trying to keep your calm during the day and going through the motions at office or school is a pain. It becomes even more frustrating to see people grumbling about lack of sleep over the weekend because they were partying till too late or watching a Star Wars marathon. People with parasomnias don’t just feel tired and sick all the time. They also feel alone and annoyed. It is very easy to mistake people with sleeping disorders as lazy or incompetent since they are almost always yawning and reaching for their cup of coffee. It is easy to assume that they love staying up until late chatting with friends or binge-watching Game of Thrones on Netflix. In reality, these are the people, who would give anything to sleep for 7 or 8 hours straight without a nightmare or sleep, terror. They would be the most grateful ones to be able to wake up one day without feeling bogged down with fatigue and pain.
People suffering from sleep disorders are anything but incompetent. They battle their disease even when they are asleep, and then, they show up for work or class as the others do. They go for days or weeks without enough sleep that the body and mind require to function correctly. The lack of proper rest compromises their immunity and cognition. They are the most likely to fall sick when the flu season hits. They are also the most susceptible to pre-examination stress.
What should you do if you have parasomnia?
If you can recognize these signs and symptoms, it is time for you to speak with a sleep expert. In all probability, a general physician does not have enough training in the nuances of sleep to diagnose you with RBD or NREM sleep disorders. You will need the help of a sleep expert now. The diagnostic procedure involves polysomnographs, EEG and sleep monitoring to rule out the secondary causes of parasomnia. There are times when doctors request patients to spend some time inside sleep clinics for proper observations and investigations. Your health insurance might cover the treatment for this, but it is always better to confirm with the agents before going in for the complete procedure.
Speak with your partner, family, and roommate. They need to know if you are in danger of hurting yourself in your sleep or if you are a potential threat to others. Giving them a heads-up will allow them to hide the keys to the front door and your car, lock your windows, check on you at night and keep their doors locked if you have the habit of roaming about in your sleep. Speaking with someone who shares your bed or apartment can relieve some amount of stress. It is bound to help you sleep a little better knowing that there is someone aware of your predicament.
There are no over-the-counter (OTC) treatments for any forms of parasomnia. Treating it requires experience, training, proper understanding of the causes and the thorough medical history of the affected individual. Cognitive behavior therapy, psychological counseling and sleep therapy help with redressal of symptoms. It is a long-term process that demands incredible patience and persistence on the part of the medical professional as well as the patient. If the causes lie in your genetic makeup, it might be impractical to hope for a permanent cure with therapy or medication, but continual behavioral therapy reduces the incidents and increases the gap between the two episodes.
The idea of someone watching you while you sleep is, at the very least, disconcerting. Now picture this: the person observing you is wearing a white coat and is located in the next room, monitoring you because it’s their duty. Even with this explanation, the situation is still rather unsettling.
The idea of sleeping on a strange bed, in a sterilized environment, possibly with monitors surrounding you, and electrodes on various parts of the body. You might wonder what good such a simulated sleeping process might bring. However, that is the standard setup for polysomnography.
What are Polysomnography and Polysomnogram?
Polysomnography translates to the observation of various stages of sleep as the subject transitions from one to another during sleep. The report of this study is a polysomnogram. It is necessary for anyone suffering from sleep-related issues to participate in one since it gives the sleep expert and your doctor a keen look at the abnormalities in brainwaves, breathing or movements during sleep. During a PSG a doctor measures the following.
- Skeletal muscle activity
- Brainwaves
- Oxygen levels in the blood
- Rate of breathing
- Palpitation levels
- Eye movement during REM
The objective of PSG is to measure the changes in the body and the brain of a subject during the transition from NREM to REM. More specifically, between the slow wave (deep) sleep and REM stage.
The Mechanics of sleep and Decoding it with Polysomnography
Polysomnography or PSG includes a complete study of biophysiological changes of sleep. Although the classic PSG study happens during the night, some laboratories accommodate shift workers, delayed sleep onset syndrome patients, and people with circadian rhythm disorders during other times of the day to study their sleep patterns.
It is a comprehensive process that considers many studies including electroencephalogram or EEG (brain activity measurement), eye movement (EOG), muscle activation and activity (EMG), and heart rhythm (ECG). After the scientific discovery of sleep apnea, breathing function tests, and respiratory effort indicators also became an integral part of the PSG test.
The Anatomy of Dreaming
Typically, REM is responsible for most of our vivid and bizarre dreams. We also experience rapid random eye movements in coordination with the visuals. The average sleeper, without any sleep-related problems, should experience about six REM cycles per night. They can switch between NREM and REM seamlessly.
It would be wrong to state that people do not dream during the NREM cycles. However, during this period, our body does not experience atonia or complete loss of muscle control. It is albeit rare. You have most likely experienced NREM dreams more than once. It is not a deep sleep state, and the sleeper wakes up easily upon slight noise or external movements.
The EEG of the brain during the Stage 2 of NREM sleep is intriguing since it shows K-complexes and high-frequency brainwaves, in short bursts. Sleep experts show increasing interest in Stage 3 of NREM sleep. In this stage, people are more likely to dream and experience parasomnias. Since this stage does not impose atonia, there is a chance that people who suffer from parasomnia move about, talk, walk, or grind their teeth while dreaming.
Earlier two distinct stages comprised stage 3, but right now the slow wave sleep and delta wave sleep occur back to back. However, people are less likely to remember their episodes of parasomnia including night terrors, sleepwalking, and sleep talking since the dreams are disjointed and less memorable.
Multi-phasic Sleep and Brainwave Studies
The vividness of dreams during the REM cycle enables us to remember them to the finest detail. The frequency of recollection of such dreams shows that most people tend to dream more during REM phases. Dreaming during the NREM stage usually occurs during the morning hours.
A comprehensive study on healthy subjects without parasomnia involved the segregation of sleep into only REM and only NREM stages. Using polysomnography and EEG, it was clear that when the subjects entered the forced NREM stage, they experienced a sub-cortical activation similar to that experienced during REM stages. That event leads to the genesis of dreams during the wee hours in the morning during regular NREM sleep as well.
Even though we have kept the explanation of NREM and REM stages brief, it is enough to understand that there are several interlinked factors at play here. Sleep is anything but the sweet release and escape into the dream world we thought it would be.
Several idiopathic disorders, secondary diseases, and external factors disrupt the quality of our nightly slumber. In fact, there are people out there, who have not experienced a good night’s sleep in years. Nightmares, night terrors, somnambulism or dream-induced movements plague their nights and keep their co-sleepers annoyed as well.
Why does Insomnia not Warrant Polysomnography?
You must remember that insomnia is the term that describes the gross lack of sleep. In cases of insomnia, people are unable to fall asleep and staying asleep. It is a complex disorder that can increase fatigue-related symptoms, decrease energy, reduce cognitive abilities and induce mood swings.
All in all, people suffering from this disorder are highly likely to feel unsatisfied with their sleep duration and quality. However, sleep experts have not noticed any kind of sleep-related abnormal behavior among insomniacs. Sometimes, the symptoms of insomnia disappear just as unannounced as they arrived. That is a classic case of acute insomnia. In other cases, the disorder persists for days, weeks and even years at times.
Once a person experiences sleepless nights for longer than three months, a doctor pronounces him an insomniac. The usual treatment can be as simple as sleeping medications, or as complex as sleeping behavior therapy, psychological counseling, and supportive medicines, depending on the cause of the disease.
In most cases, chronic insomnia is comorbid, i.e., it occurs as a side effect of other disorders like high blood pressure, hyperthyroidism, dyspepsia, depression, and bipolar disorders. Therefore, the treatment of it is more complicated than acute insomnia. Your sleep specialist will need to speak with you in detail about your sleeping habits, recurrence of sleeplessness, history of insomnia in the family, and discuss the treatment plan in detail.
What is the Necessity of Polysomnography?
As you can understand from this, the inability to fall asleep at a socially acceptable time, remain asleep for the desired duration and waking up earlier than desirable can qualify as insomnia. The signs of insomnia are quite visible, and doctors can find out if you have it once they start learning about your daily habits, including bouts of sleeplessness and sudden awakenings during the night. Diagnosis of it usually does not require sophisticated, comprehensive testing like PSG. Even the usual complaint of fatigue does not demand a PSG.
A comprehensive set of tests like the ones that make up PSG are typically used for the detection of the more complex interlink of disorders including restless legs syndrome (RLS) or periodic limb movement disorder (PLMD), narcolepsy, idiopathic hypersomnia, idiopathic parasomnia, REM sleep behavior disorder (RBD), and sleep apnea. These disorders are quite complicated since they involve multiple stages of sleep, or they are the result of the discomfort caused by secondary diseases of the body.
Although doctors do not run PSGs on people complaining about circadian rhythm disorders, this test can rule out the ones as mentioned earlier. That is a method of detection by the rule of elimination.
What is the Mechanism of a Standard Polysomnogram Test?
The setup and mechanism of the process are quite complicated. A polysomnogram will include the recording of minimum 12 channels. That would require a 22-wire attachment to the patient. The number of channels and wires will vary between two laboratories.
The preference of the doctors will determine the nature of the channels and the placement of the wires. Here’s a brief idea about the minimum number of channel requirements and their purposes.
- Three channels for EEG.
- Two channels measure the eye movements during the EOG.
- The number of channels can vary between one and two for the airflow measurement.
- A doctor may recommend one or two channels for the study of chin muscle tone.
- At least one muscle measures the leg tone.
- Minimum one lead measures the heart rate and palpitation.
- The belts require one channel each since they measure the chest wall and upper abdominal wall movement.
- One channel measures the saturation of oxygen.
All of them accounts for the minimum 12 channel requirements in every sleep clinic.
In most cases, the piezoelectric sensors measure the movement of the belts. Sometimes, respiratory inductance plethysmography replaces these sensors for the same purpose. The action produces low-frequency waveforms as per the inhalation and exhalation. It is possible for this method to give rise to artifacts, especially during the study of obstructive apnea cases.
What are the Critical Parts of a Polysomnogram?
Each channel has multiple connecting wires that lead to the central box. The central box has a direct connection with the computer that displays, records, analyses, and stores relevant patient sleep data. When the subject is asleep, the monitor displays data sets from several channels simultaneously.
Most sleep clinics and laboratories have small video cameras in the sleeping chamber that can observe the patient’s movements and convey their dialogs during sleep-talking to the next room. It is a wholesome system that accounts for all sorts of physical and physiological changes during the patient’s slumber.
Measurement of Brain Activity with EEG
The standard EEG process uses six exploring electrodes. It also employs two reference electrodes, unless the doctors suspect a seizure disorder. In the event of a seizure during sleep, more wires are necessary to monitor brainwave activity. These exploring electrodes go on the possible frontal, central , and occipital regions of the skull. The paste that holds these electrodes in place will conduct the electric impulses that originate from the neurons of the cranial cortex.
These exploring electrodes send the signal according to brain activity that represents different stages of sleep. An expert can easily tell these signals apart depending on which stages they belong. EEG helps in studying the brain activity of the different N1, N2, N3 (NREM) and REM stages of sleep.
EOG Measures the Electric impulses of the Eye Movements
The electrooculogram (EOG) measures the extent of eye movement during the REM sleep. This process uses two electrodes. The expert places them about 1 cm above the outer corner and 1 cm below the lower edge of the right and left eyes respectively. Each electrode picks up on ocular activity. It is possible to detect something as minute and delicate due to the subtle potential difference between the retina and cornea (the latter has a positive charge).
When REM sleep occurs, there is rapid eye movement that alters the potential difference and sends electric signals across through these leads. Therefore, the observers can quickly tell when REM sleep begins and how long it extends.
EMG monitors the Skeleton-muscular Activity
While studying the quality and quantity of sleep, there is no way one can miss out on the study of muscle activation. The classic definition of REM states that during this period, there is a complete loss of muscle activity or the onset of atonia.
NREM period does not have atonia, and it is possible for people to move their body during the N1, N2, and N3 stages. However, people with periodic limb movement disorders and RLS can move their legs even when they are fast asleep. There are several instances when a person has been able to move his or her legs (and sometimes their hands) during sleep.
Such situations indicate abnormal muscle tension that should not have been present during this stage of sleep in the first place. Ever since we were children, we have associated rest with relaxation. It is not wrong to believe that sleep involves complete relaxation of muscles. In fact, when you dream of running behind another person, the only reason we do not run in our real life is that we lose complete control of our muscular activity. You could think of it as partial paralysis unless the person suffers from REM behavior disorder (RBD). In RBD, a person can talk, sit up, walk around, eat and even hit others during his or her sleep.
ECG or EKG Observes the Heart Activity During a PSG
A standard ECG procedure involves ten electrodes. Polysomnogram uses only about two or three for the entire process. The medical professionals usually place one wire under the collarbone, on each side, and one about six inches above the waist on the left and one on the right.
As the heart goes through its systolic and diastolic motions, these electrodes measure the movement. The result is in the form of a graphic wave that has distinguishing features like the P wave, QRS complex, and the T wave. The duration of each motion translates as the troughs and crests on the electrocardiogram.
Any abnormalities in the structure of the wave corresponds to the irregularity in the heart function. Since each node denotes a particular feature of the heart, doctors can figure out the underlying pathology from the ECG.
Measurement of Respiratory Factors
The analysis of oral and nasal airflow is crucial during sleep. People, who sleep soundly, usually do not snore much. On the other hand, people suffering from breathing obstruction can feel discomfort that results in snoring and vocalization (groaning) during sleep.
A pressure transducer usually measures the rate of oral and nasal airflow. The clinician can easily estimate the rates of respiration from this data. Sometimes, patients resort to mouth breathing when there is an obstruction in their nasal airway. It can produce false negatives and often leads to misdiagnosis. When the condition is obstructive apnea, clinicians can identify it as hypopnea.
What do the Experts Record During a PSG?
Video and audio recording serve as sound sources of information about the patient’s breathing and respiration. It is especially useful in studying sleep apnea among patients. A sleep technician can note the snoring problem as moderate, mild, or loud depending on the loudness and frequency of snoring. They usually use a numerical scale of 1 to 10 to do so. Snoring results from blockage of airflow and it can state whether the hypopnea can be obstructive sleep apnea (OSA).
A combination of the results from the numerable tests that form the cohesive PSG process eliminates the possibility of artifacts in the outcome. Misdiagnosis is a distant possibility when there is not enough data from the personal observation of the doctors from videos and audios of the sleeper.
What should I Prepare for During my first Polysomnogram?
In general, the patient needs to come to the sleep clinic. It can be a private clinic or a hospital. The patient needs to go in early (preferably the same evening), so the doctors and clinicians can hook up the channels and wires. Sometimes, the clinicians will recommend a hotel that has facilities to set up sleep studies and allow cameras in the room so that the experts next door can keep an eye on the patient’s sleeping habits.
It takes some time for the patient to get used to the wires and channels. However, you must remember that sleep apnea studies are also typical among children as young as 3 years old. Therefore, it is a safe procedure, and the location only serves the purpose of comfort and not health or safety.
Sometimes, in critical cases, when the patient has shown several artifacts in previous test results, the clinicians may agree to set up the entire mechanism at the home of the patient, where he or she can be a little more comfortable than inside an artificial environment.
Typically, a person sleeps through the night with the wires hooked on to the monitors that generate regular graphs and data. Additionally, the clinicians observe the movements and listen to the snoring tendencies of the participant every second. The patient can usually go home the next morning. However, if the clinician recommends a sleep latency test or excessive daytime sleepiness (EDS) test for the patient, he or she might have to stay another day.
What Does a typical PSG report State?
Once the test is over, the scorer completes data analysis by converting the data into 30-second periods. You can get the following data from any such score.
- Sleep onset latency. It is the time a person takes to fall asleep after the lights go out. The average sleep latency is around 20 minutes or less for the ordinary person. The interpretation of their sleep-wake state depends upon the patient’s EEG results and not on their personal encounters.
- The efficiency of sleep. How well did the patient sleep? The usual method of determining it is through dividing the number of minutes of rest by the minutes in bed. The efficiency score usually lies between 85% and 90%. For some sound sleepers, it is even higher than 90%.
- The different stages of sleep. We know by now that rest has four main stages – N1, N2, N3, and REM. The information on the sleep stages of a patient comes from the seven channels connecting EEG, EOG, and EMG. This data is enough to determine how a person transitions from NREM to REM stages. It will show how long a person spends in light sleep, delta sleep, slow wave sleep, and REM. While the fraction of time in each stage depends on the age, there are other factors like health, obesity, blood glucose, anti-depressants, pain medication, and antipsychotics that can contribute to aberrations in the result.
- Breathing difficulties during sleep. Breathing irregularities can arise from many factors. Smokers, people prone to allergic rhinitis, simple cough and cold, and bronchitis can all contribute to breathing difficulties. Sleep apnea is different from any of those. It is the complete blockage of breathing for at least 10 seconds that lead to desaturation of oxygen from the lungs. The previous cases we have discussed result in 30% or lesser airflow that can lead to awakening.
- Sudden awakenings or arousals. We have all experienced this at least once. We have found ourselves wide awake in the middle of the night with no idea what woke us up, or we have woken up confused and gone back to sleep. These can happen due to many reasons including sudden limb movements, environmental noises, and breathing difficulties.
The other information comes from the movement of the subject in his sleep, the levels of oxygen saturation in his lungs, the cardiac function and rhythms, and the preferred position of the patient.
Once the data is complete and the clinician has scored it based on his observations, they go to the sleep expert. The diagnosis is a complicated process since the medical professional has to take account of the previous medical history, current medication, history of drug and alcohol abuse, family history of insomnia and other health-related information.
Do I Need Polysomnography?
The only person fit to answer that question is your GP and sleep specialist. Sometimes, problems like abnormal movements during sleep that range from pure kicking and punching to the more complex sleep-sex can disrupt regular rest. Apart from lowering the quality of sleep, these symptoms also disturb the life of a couple and disrupt the relationship between roommates.
If you are experiencing any of the following symptoms below, you should speak with your medical expert immediately.
- Restlessness during sleep.
- Holding your breath during sleep and waking up for large gasps of air.
- Excessive sleepiness during the daytime followed by poor quality sleep at night.
- Loud snoring that occurs throughout the night.
- Waking up multiple times during the night with or without valid cause.
These signs can be of narcolepsy, parasomnia, REM behavior disorder, sleep-related seizure disorders, and “sleep attacks” during the day, and continuing discomfort during the day. The latter can prompt the patient to move their legs frequently to reduce the tingling, crawling and burning sensation in their legs.
Sometimes, this kind of discomfort can also attack the upper limbs. RLS occurs in males more commonly than females, although it usually begins in the late middle-ages. Consumption of alcohol, regular intake of anti-depressants and antipsychotic medication, and a history of drug abuse increase the propensity of sleeping disorders. If you identify with one or multiple of these signs and symptoms, you need to seek counsel of a sleep expert.
What are the Risks Associated with PSG?
Children and adults have to undergo PSG from time to time if they complain about recurrent sleep-related issues. It is a non-invasive process that is painless. The nodes attach to various parts of the forehead, neck, chest, and face via a conductive adhesive. The only risk is irritation from the adhesive. However, that goes away quickly with soothing ointments and anti-histamines topically.
What can be the Possible Interpretations of the Result?
Interpreting a PSG report is not a layman’s job. Even if you are curious and you absolutely need to Google the findings, do not rely on your understanding or interpretation skills completely to start treatment or stop the ongoing medication. A team of medical experts including physiologists, sleep experts, and psychologists need to work hand-in-hand to interpret the results of the PSG.
In case you find an abnormality in the results, you might see the following;
- Breathing disorders that can be the early signs of sleep apnea.
- Abnormal daytime sleepiness that can lead up to narcolepsy.
- Movement disorders that can be a secondary pathological condition or complex idiopathic RLS or PLMD.
- Seizures during sleep that are otherwise hidden and not felt by the patient.
The medical experts need to take a look at your complete breathing and hypopnea profile to determine the chances of you having sleep apnea. The data helps them measure the apnea-hypopnea index (AHI).
What’s the next step After Receiving a PSG Report?
After you get a PSG report, your doctor might state that you have sleep apnea. Since the inference relies on several inclusive and exclusive studies including the AHI studies, there is a reason to believe that you might require a sleeping aid regularly.
Something like a continuous positive airway pressure (CPAP) machine can help you maintain proper pressure in the airway. It will provide complete air supply to your mouth or nose. Even when you are asleep, the CPAP machine will continue to supply positive air pressure to your respiratory tract, so your breathing remains smooth.
To find the correct CPAP setting, another polysomnography might be necessary. The recommendation depends on your adjustment to the initial CPAP settings, the prognosis, level of improvement and the recommendations of the doctor.
What Should I Remember About Polysomnography?
Just like every other medical test and procedure, you need to learn and remember a few facts about PSG.
- It is a test that will generally happen in a clinic or hospital setting. However, upon special request, some professionals set up their machinery and monitors at hotels and homes.
- PSG is undoubtedly non-invasive and entirely painless, but for the first timers, falling asleep with uncountable leads on their body can be uncomfortable.
- You should refrain from drugs, alcohol, and smoke for 24 hours before your PSG.
- The sleep doctors will monitor your brain activity, heart rate, eye movement rate, and muscle activation rate and blood oxygen while you sleep. It is necessary that you go in at least an hour before your appointment to assist them with the preparation.
- You should focus on packing things that define your bedtime routines like your favorite set of pajamas, your eye mask, maybe a snuggie too. Each clinic has its prerequisites and rule. You need to speak with the doctors about what is permitted and what is necessary.
- Remember not to drink caffeine for a couple of hours before the surgery. It can interfere with the slow wave and delta wave readings.
PSG is anything but a simple procedure for the doctors and clinicians to run, but it is indeed simple on the part of the patient. The person needs to act normal and go the sleep at his regular bedtime, so the experts can sit and monitor the different sleep indicators from the next room.
What’s your secret to catching some Z’s every day? Do you dive into a solid 8-hour slumber when night falls? Or maybe you sneak in some shut-eye in the afternoon, or grab a quick nap at your desk during a break? Could it be that cozy pre-dinner nap on the couch is more your style? Your snoozing routine pins down what kind of sleeper you are.
Most of us crave a long eight-hour stretch of sleep. We wait for days on end to be able to get in bed by 11 pm and sleep till 7 am without any interruptions. However, how many among us can achieve it? Over 70% of the American adults are sleep deprived, and it is impossible to catch up during the weekend due to specific commitments that include their children’s soccer practice, extra lessons, weekend parties, social plans, and work from home schedules.
Naps are not Only for Toddlers Anymore
The thought of not getting enough sleep due to work makes us want to go back to our childhood when we had the luxury to deny a nap. What wouldn’t we give to go back to bed in the afternoons or sleep in on Saturday mornings? Alas, that is not an option!
Aside from hitching a ride on a time machine, the only other option is to adopt a more flexible sleeping schedule. It is evident from several research publications that it is possible to divide a night’s rest to multiple parts. It might not even be necessary for the sleeper to spend eight hours in bed every night. Such deliberately fragmented sleep is now famous as polyphasic sleep.
How can you Sleep less Without Feeling Sleep Deprived?
You are likely to think that polyphasic sleep schedules promote sleep deprivation and you are better off with the meager five hours you are getting each night. However, accounts of the veteran Everyman and Uberman sleepers show that it is possible to sleep for only about two to three hours a day and still feel completely rejuvenated.
The objective of complete rest is the replenishment of physical energy and mental health. Sleep deprivation does a number on the physical integrity and mental health. Cases of depression, bipolar disorder, anxiety disorder, and schizophrenia worsen with the persistent lack of sleep.
Moreover, the concept of catching up on sleep during the weekends turns out to be a myth. Regular slow-wave sleep and REM are essential to keep you sharp and functional for the next 24-hours.
How Does the Practice of Resting in Segments Changed Over the Years?
Polyphasic sleep has developed, evolved, adapted and mutated over the last couple of decades. It is difficult to lay your finger on a single type of fragmented sleep schedule that works universally well. Rest is an individual requirement, and you need to have a thorough understanding of your body, mind and sleep habits to find a schedule that fits your bill.
Polyphasic sleep comes in many packages like the Dymaxion sleep, Uberman and Everyman schedules. You will find multiple well-known patrons of each practice. Each sleeping schedule has distinct objectives. However, almost all of these schedules have one common goal – to increase waking hours and yet complete REM sleep every day.
The concept gained popularity through holding the hands of Dr. Claudio Stampi, an Italian chronobiologist. His work focused on the effects of light and dark on the human body. Speaking in more scientific terms, he studied the sleep-wake cycle in humans and its impact on the functions of different organ systems.
How do our Genes tell Time?
In reality, human beings have multiple genes that act as the internal clock. These clock genes respond to natural light to “tell” the time to the body. According to the response of these genes, the melatonin levels in our bodies fluctuate. It is a neurohormone that signals the brain when it is time to fall asleep and when it’s time to leave the bed.
Depending on its concentration we either feel worn, tired and droopy, or we feel active, awake, and alert. As you can expect the hormone levels are highest during the night, it peaks at around 3 am and then begins to decline. Going into deeper sleep means fast degeneration of this hormone by a natural process. The lack of enough sleep causes the buildup of melatonin, and that makes people sleepier and sloppier than usual.
It is understandable that almost all sleeping schedules aim at providing necessary slow-wave and REM stages to all sleepers. That should help in rapid degeneration of this hormone irrespective of the duration of rest and prepare the person for his or her daily hurdles. That again brings us back to the point that the physiological necessities of two people can never be identical.
Therefore, there is no way someone can dictate which sleeping schedule is ideal for you. Sometimes, we wish that picking one would be as simple as choosing a swimsuit or a pair of oxfords, but the reality is rarely rosy. So, you will have to go through the intense exaptation, adaptation, and observation period for everyone in these schedules.
How Does Evolution Support the Theory of Segmented Sleep?
Extensive research on evolution and adaptation shows that all human ancestors are either biphasic or polyphasic sleepers. Generally, humans are supposed to stick to a polyphasic or biphasic sleep pattern. However, we have adapted a monophasic routine due to the social construct.
The nature of the daily school, university classes and office support continuous six to eight hours of sleep. Most offices do not have nap rooms and even think about catching a nap in a Manhattan office seems too bizarre. Only a handful of companies in Japan, few startups in the US, and a couple of colleges are trying to bring the practice of naps to the mainstream.
The history of polyphasic sleep is not ancient unless you consider the possibility of our cave-dwelling ancestors living life on exclusively polyphasic resting systems. Their nature of hunting-gathering lifestyle would only flourish in the presence of fragmented sleep.
However, anthropologists and biologists have not found much evidence on similar sleeping habits among human ancestors who evolved after the cavemen. Since not much is there that can point towards the sustainability of the practice or the possible ill effects of it, thought leaders like Buckminster Fuller have had to experiment with polyphasic sleep throughout their lives to prove its effects.
Slumbers, Naps and Wakefulness Stimulants: an Account of the most Popular Polyphasic Sleepers
While talking about Buckminster Fuller, we cannot disregard the Dymaxion sleep schedule. It is one of Fuller’s most controversial, yet greattest legacy. People have hailed it as one of the most formidable polyphasic sleep schedules, but if you manage to perfect it just as Fuller did, you might be able to go through life with as little as 2 hours of sleep per day.
Unlike Voltaire and Balzac, Fuller has never been famous for his particular fondness for caffeine. Nonetheless, he managed to pull several all-nighters, deliver speeches, and attend inaugurations in the morning. His secret was a strict but bizarre sleeping schedule that he referred to as the Dymaxion sleep.
The name comes from the portmanteau of – dynamic, maximum and tension. It reflects the perseverance, tenacity, and courage with which he practiced this foreboding schedule on himself. On several occasions, he has stated that two hours per day was more than enough sleep for him. He explained that each human being has an inherent reserve of energy.
We rarely ever run out of it, but we do need to replenish it. Think of it as topping off a drink, when you still have a bit left. According to his observation and theorization, we should stop and take a nap at the first sign of tedium. That should top our energy reserve off before it hits rock bottom. Napping for 20 minutes or 30 minutes should be enough.
Napping from time to time instead of engaging in full-fledged sleep is sometimes more than enough. We have all experienced this either during our high school years or in college between classes. Catching a quick shuteye can make us feel renewed and wipe away the fatigue entirely.
When someone can manage to nap for 20 minutes every 4 hours, he or she can eliminate the need for eight-hour sleep. They would spend only about 2 hours per day asleep and have 6 hours more to kindle his hobbies and passion. Power naps are the secret weapons that will help you go through a day without feeling drowsy, confused and irritable. At the end of the year, you will have added over two months (or 3 months depending on the schedule you follow) to a year.
People new to polyphasic sleep will face considerable challenges adopting a new and rather strange routine of power naps that replace long stretches of nightly sleep. However, it is a great blessing for the night lovers, who love to stay up until late working, playing music, reading or just watching their favorite show. No matter how intriguing the prospects of gaining close to 6 extra hours per day are, people need more than external motivation to plow through weeks and months with about two to three hours of sleep per day.
In such cases, mobile applications dedicated to controlling fragmented sleep can be beneficial. Smartphone applications like these usually have alarm settings, immersive activity settings, exaptation and adaptation planning schedules for the beginners. They also come with an extensive database of knowledge on the pros and cons of the popular polyphasic resting practices.
Some evolved smartphone applications can collect the relevant data about your slow-wave sleep activity and sleep quality. You will get a detailed look into your sleep statistics, and that will give you a clear idea about the duration of rest you need and the frequency of these naps.
Several wearable gadgets have also started polyphasic sleeping scheduling. These are effective ways to bail on endless slumbers and adopt a more time-budgeted resting routine for your daily boost of energy. There are simpler versions of these applications as well, that can give you a visual guide for the onset and offset of sleep. You can input the time you need to wake up in the morning, and the calculator will tell you the exact distribution of your nap times throughout the day and night.
Is Segmented Sleep the same as Polyphasic Sleep?
Segmented sleep is not always synonymous with polyphasic sleep. In most places, segmented sleep refers to different forms of biphasic sleep. When we say different types, we refer to the two most common forms – siesta sleep and equally distributed segmented sleep at night.
Siesta
Siesta refers to an hour or hour-and-a-half of afternoon sleep. Most people in the US might not be aware of it, but it is a prevalent practice among the residents of Spain and other Southeast Asian countries to take a short nap in the afternoon.
If you visit Spain, you will notice that their shops and other businesses remain closed for at least 2 hours in the afternoon. That is the time the operators and owners go for lunch and sneak in some quick rest before returning to their business in the early evenings.
The same is true for shops and trades in India, Bangladesh, and a few companies in Japan. Siesta boosts the energy reserve so that the people can return to work with renewed vigor. The afternoon nap is a common practice for the hotter climates where business is rather slow, post noon.
Equally Segmented Sleep
You might not find this in popular practice right now. However, historians and behaviorists suggest that it was a common practice in 15th and 16th century France. People would go to bed early, then wake up at around 2 am for prayers, writing journals, reading books, studying or sex, then go back to bed at approximately 4 am. They slept in two equal fragments of four hours each.
Philosophers and religious bodies believed that the two hours in between the resting periods was conducive to creativity. This sleeping behavior depended on the local lighting patterns, times of sunset and sunrise, and the adopted behavior of the region. The segmented sleeper got between 6 hours and 8 hours of sleep per day.
Triphasic Sleep: The Underdog of Polyphasic Sleep
Triphasic sleep is something we don’t hear about much. It is indeed a form of polyphasic sleep since it involves more than two separate segments. Life made this sleeping popular among the millennials.
While it is a little odd as compared to the biphasic patterns, it is also quite simple. The exaptation process is almost nil in this practice. Even without it, the adaptation only takes a couple of days. Once you manage to master your triphasic resting routine, you can expect to gain about three to five hours more per day.
Next, we finally enter the realm of the much-feared and much-admired polyphasic sleep. Polyphasic patterns can have various types and subtypes depending on the duration of the breaks and naps. Each model has a different objective, but they contribute to several extra hours of wakefulness per sleeper.
What is the Everyman Schedule?
First, let us try to understand the everyman 3 schedule. Puredoxyk came up with the idea and the name, right after the coined Uberman. The everyman schedule has changed quite a bit since people first started practicing it. The original plan involved a three-hour core and three repetitions of twenty-minute naps.
These napping sessions correspond to the crests of alertness that naturally occur throughout the day. The circadian rhythm and ultradian rhythm keep us swinging on the highs and lows of sharpness in a twenty-four-hour period.
Our retina acts as photoreceptors for our circadian clock genes. With the help of them in coalition with our liver, our body can determine the time of the day relatively easily. The slow-wave-sleep pressure increases between 3 pm and midnight. Then the REM pressure increases from 3 am to about noon.
Therefore, you are likely to experience a better-quality core sleep in the evening and morning core is not going to be restorative at all. When you hit the hay around dusk, your chance of getting proper delta sleep is much higher than napping in the morning. As a result, the 3.5-hour core is more suitable than 3-hour core sleep for most people.
Here’s a very regular everyman schedule you can try if you are new at it.
- Core sleep: 9 pm to 12:30 am
- Nap: 4:10 am
- Nap: 8:10 am
- Nap: 2:40 pm
As you can see here, the core sleep duration is perfectly 3.5-hours, and it is during the dusk. Now, a lot of people might ask if it is at all possible to fall asleep by the clock since timing is of great importance here.
Well, it takes a little time to get used to. No everyman sleeper could perfect their schedule at one go. It takes numerous errors and missed alarms to be able to gain those six extra hours per day.
How to Avoid the Zombie-mode During the Everyman Adaptation?
According to several everyman followers, setting two alarms during your exaptation phase can help you. You should always place them at 3-hours and 3.5-hours respectively. It will prevent you from entering the most dreaded zombie-mode during the daytime when you have work to do.
Restricting the core to a couple of hours within dusk should do the trick. On the weekends, you can push it back an hour or two. It is significantly more effective than going to bed late every day.
What is the Uberman Sleep?
Next, we come to the favorite Uberman schedule. Puredoxyk coined this term as well, and quite honestly, this schedule is ideal for the ‘Ubermen’ we see around. It consists of six evenly spaced 20-minute naps throughout the day.
Now, there is not much data on the health implications of this schedule, but it is safe to say that not everyone can quickly adapt to this one. Adjusting to a biphasic or triphasic sleep is much more comfortable than practicing the Uberman sleep. Although, you will find several accounts of “Ubermen,” who have successfully done this for over a year or two. By far, these people have not reported any adverse effects to this practice.
Apart from indomitable determination, you will require a human alarm system to follow this sleeping pattern. Without external help, it is almost impossible to wake up after 20 minutes of rest and to work for close to 3.5-hours, and nap for another 20 minutes.
How to Overcome the Primary Challenges of the Uberman?
The most testing part of the Uberman schedule is the exaptation process. It requires the sleeper to remain awake for a stretch of 24 hours to 36 hours.
According to the experts, who have done this before, after this initial phase of staying awake, you will feel a “second wind” or a fresh burst of energy? That is when you should try to catch your first 20-minute nap. At this point, you should start taking such naps every 2 hours or so for the next 4-5 days. That should regularize your REM stages so that each resting phase corresponds with REM.
Adaptation without exaptation is not a good idea for anyone. Even if you are a diagnosed insomniac, you should first try the exaptation before moving to the next step. You should nap every 3 to 4-hour interval. Exaptation can prevent the infamous “zombie-mode” from setting in. It might take you between 3 weeks to 4 weeks to adapt to this schedule. However, some people take significantly longer. Even when you feel that these 20-minute rests have become the norm for you, your body will continue to adjust to this new schedule for months.
Why is the Uberman Schedule Demanding for Most?
Before you jump on board thinking about the five long hours of extra time you will get when you manage to adopt this routine, you should think about the feasibility of the method.
Science states that the necessity of rest per individual depends on their genetic makeup. Only about 5% of the people in the world can survive healthily and remain completely functional with only five to six hours of sleep. That means lesser than that 5% can get by with only naps throughout the 24 hours.
There’s another way to minimize the challenges the equidistant Uberman with 6-naps puts forth. You can try resting for longer at night. That is a form of non-equidistant Uberman, and it escapes the SWS crash the traditional Uberman faces.
Taking longer naps of 40 minutes instead of two short 20-minute naps can help your brain transition into REM from SWS in a natural rhythm. According to the new Uberman variants, you can indulge in longer naps at dusk.
What’s the Dymaxion Sleep Schedule?
The Dymaxion schedule has been trending for the last two decades. Buckminster Fuller made this schedule a part of his legacy. He was famous for not sleeping much and indulging in several fields of work at the same time.
He stated that he found all the extra time from the practice of this fantastic schedule. However, recent research shows that people with one or multiple active copies of the DEC2 gene can successfully attempt the Dymaxion. Sadly, that means only 1% of the world’s population can succeed at it.
It is a bit more controversial than the Uberman although it has identical sleep-wake hours. It lacks some of the significant advantages of the Uberman and Everyman schedules. Thus, not a lot of netizens have found it as enticing or practical. In the case of the Uberman, the sleeper can enjoy a frequency advantage. That means he or she can frequently get the much-required REM sleep when he or she shuts the central unit down.
It reduces the sleep pressure. On the other hand, Dymaxion sleep encourages less frequent REM sleep, and it is not as practical (or user-friendly) as the other ones. There is a large chunk of REM and lesser frequent REM naps. It does not dissipate the building sleep pressure. The chances of sleep deprivation and crashing are significantly more with Dymaxion than it is with Uberman. The fatigue buildup for any Dymaxion sleeper may be a lot higher than Everyman and Uberman sleepers.
What is so Great about the Dymaxion Sleeping Schedule?
As per the notes and practices of Buckminster Fuller, the founder of Dymaxion sleep, it should ideally consist of 4 equidistant naps for 30 minutes. It translates to about 2 hours of sleep per day only.
Just like the other well-known proponents of equidistant naps like Salvador Dali, Leonardo da Vinci and Edison, Fuller never felt bogged down by fatigue during the daytime. He was an inventor, thought leader, and entrepreneur, who was always on his toes. Fuller had mentioned it several times that sacrificing regular 7 to 8-hour sleep had helped him stoke his creativity. As a result, he was never bored and never tired.
Modern followers of Fuller’s theories have developed new Dymaxion routines that are more realistic than the previous one. It pays heed to the increase in sleep pressure and the requirement of SWS sleep after dusk. Therefore, instead of practicing four equidistant half-an-hour naps, the neo-Dymaxion sleepers adopted a routine that allowed 1.5 hours of sleep during the nightfall, a 30-minute nap in the morning and afternoon, and a 20-minute nap in the evening.
Why should you speak with someone before starting your new sleep schedule?
So far, you have seen the personalization and adjustment of several popular polyphasic schedules according to the convenience of the sleeper. You should never attempt a new program because of your significant other, friends or family member is trying it. On the other hand, when you share the fact that you might be seeking a new sleeping schedule that involves short bursts of naps instead of long sleeping hours, your family and friends will try to talk you out of it. It is imperative that you have enough information about the kind of polyphasic schedule you are working on to convince them. You need at least someone by your side to help you during the exaptation and adaptation process. Adapting a new schedule is impossible with eye masks and alarms alone. You need human help (can be a parent, friend or SO).
What should you always consider before attempting controlled fragmentation of sleeping hours?
You must remember that staying awake for the first 48 hours is not even the beginning of the challenge. Yes, it has been possible for super-humans like Randy Gardner and Peter Tripp to stay awake for over 11 days and eight days to set world records in 1965 and 1859 respectively, but for the most of us, it is impossible to stay up all night studying, give an exam, and party all night. Staying up for over 24-hours is enough to send us into the zombie-mode. When doctors monitored the heart rates and brain waves during these phases, they discovered some staggering (but quite expected facts) –
- The core temperature falls below normal
- The heart rate increases
- Blood pressure increases
- Alertness drops
- Melatonin levels are on the rise
- Cortisol levels are on the rise
- Immune cell activity falls
- Motor activity reduces
Several other measurable parameters change due to the lack of enough sleep. Therefore, throughout the exaptation and adaptation process, when you are experiencing some form of sleep deprivation, you will face these challenges consistently.
People who have undergone major surgeries in the recent past, patients recovering from viral infections, children and teenagers, those with high blood glucose levels or hypoglycemia, persons suffering from and blood pressure irregularities should never attempt polyphasic sleep. If you have any sleeping disorder, including insomnia, advanced sleep phase or delayed sleep phase syndrome, do not practice fragmented sleep.
Biphasic sleep might be a good idea for them though since a siesta can help them feel fresh, rested and it can boost the healing mechanisms in the body. Taking an afternoon nap also takes care of the leftover melatonin levels. Additionally, if you are taking prescription pain management medications, a short nap in the afternoon will take care of the sleep-inducing properties of the medicines.
Sleep is commonly linked with rest, lazy Sundays, and unexpected free days that encourage us to stay in bed a bit more than usual. It has turned into a preferred activity for numerous adults, who … Read more
Sleep is commonly linked with rest, lazy Sundays, and unexpected free days that encourage us to stay in bed a bit more than usual. It has turned into a preferred activity for numerous adults, who rarely get the chance to take a break from their work and multiple duties. Remember how, when we were kids, our parents had to exert effort to persuade us to nap in the afternoon? It is only in hindsight that we realize the valuable chance we overlooked to delight in afternoon siestas.
Today, adults crave the opportunity to grab some much-deserved rest during the day and night, before it’s time to start the rat race once again. Sleep has become a precious commodity that pharmaceuticals sell in expensive bottles.
According to a study, over 70% of the US adults do not get enough sleep. Some of them wake up repeatedly due to recurring nightmares, breathing difficulties, leg cramps, and associated problems. Most of the rest deprived souls believe that they will be able to catch up on sleep “the next weekend.” Adults, teenagers, and young kids are victims of deliberate sleep deprivation.
It starts out as something innocent and manageable, but with constant abuse of resting schedules, it takes only a couple of months to become a sleeping disorder.
What Should You Know about REM Stages of Sleep?
Proper rest is significant for every mammal with a brain structure similar to their human friends. In fact, the structure of sleep is conserved among higher mammals. According to human sleep studies, regular rest consists of several stages. It is not as simple as falling asleep and dreaming about Zac Efron until you wake up.
Even a child’s rest has multiple complicated steps. However, the distribution of the stages varies as a child grows up into an adult. Infants and toddlers experience about 80% of their sleep time in the REM stage. Adults only spend about 20% to 25% in REM (Random Eye Movement) sleep.
As you drift off to sleep each night, your brain enters the NREM (non-REM) sleep stages first. After four such NREM stages, the mind enters the REM stage. Some people even begin dreaming almost immediately after falling asleep. However, dreams during the REM stage are unique.
These dreams are more vivid than others, and rapid intermittent eye movements accompany these images. Research shows that these linear movements of our eyes may have something to do with the vivid images that our brain conjures. Studies also link these image formations with memory construction. Without enough REM sleep, it would be impossible for anyone to remember and recollect details correctly.
Interestingly, the REM stages increase in duration as we reach waking time. Each successive phase is longer than the previous one. Scientists have studied the intensity and extent of each period through electrooculography (EOG). This process measures the rate and scope of the movements of the eyes.
Observation of several REM sleep study subjects shows us that the action is intermittent and not constant. The eye movement during the REM stages has a direct relationship with dreams and memories. However, their exact function is still a mystery to modern sleep study experts. REM also show a significant correlation with spikes in the brain wave activity, and they have direct links with the stimulation of the visual cortexes of the brain.
Why do Experts call REM “Paradoxical Sleep”?
The brain wave during REM is typically slow. It is a part of the slow wave activity that characterizes restorative sleep. They consist of low-amplitude, mixed-frequency brain waves. Experts often refer to this stage of sleep as paradoxical since its brainwave activity is very similar to the waking stage of a human being.
Sawtooth waves comprise the wave activity of REM sleep.
Beta waves, alpha waves and theta waves make up the total wave composition that reflects a high level of energy consumption and oxygen take-up. As a result, the rate of respiration during this stage increases and almost reaches that of wakefulness. The core temperature reaches ambient temperature, and blood pressure tends to increase as well.
These factors can help explain why people face difficulty in entering REM with sleep apnea and associated sleep disorders. The increasing rates of oxygen consumption lead to rapid breathing. People suffering from sleep apnea, without CPAP assistance ( Continuous Positive Airway Pressure ), risk breathing difficulties when they enter paradoxical sleep. Our muscles tend to relax when we are asleep, but during REM, we lose complete control over our muscles.
Neurologists and sleep experts often compare this to paralysis and atonia. The part of the brain that sends impulses to the muscular neurons experiences complete suppression. Only those that control ocular movement, breathing, circulation and diaphragm rhythms remain active. The beginning of this suppression mechanism occurs at the pons via the release of norepinephrine.
At a neurological level, REM sleep begins with the secretion of acetylcholine. The levels of this neurotransmitter remain high during wakefulness and REM sleep. It makes neurologists believe that acetylcholine is imperative for memory formation. An acute deficiency of acetylcholine points towards difficulties in memory formation and information retention.
Serotonin or the happy hormone in our brains have the power to inhibit proper restorative sleep. People with serotonin-dependent depressive disorders often experience severe challenges in meeting their daily REM requisition. In fact, surgical elimination of serotonin production sites can eliminate REM sleep. It shows that acetylcholine activation and norepinephrine secretion are not enough to begin the REM stage. Complete deactivation of “wakefulness” is mandatory for REM.
How is REM sleep a contradiction of its own?
Learning the mechanisms of REM sleep is not the confusing part. Finding out what the lack of it does to people is. Numerous studies show that the lack of it has a handful of effects on complex human behavior. People, who do not get enough restorative sleep for days on end show impaired learning, compromised memory and the ability to complete complex tasks. Such profound effects may be characteristic of chronic sleep apnea, but for most parts of the population, these effects are much less intense. Our brains have an exceptional rebound mechanism that can make up for the lost REM activity. When you do not experience enough REM sleep during successive nights of rest, your brain enters a state of rebound REM.
The original duration of a REM stage is between 90 minutes and 120 minutes. During rebound REM, the period can increase by about 20%. A rebound state may be as long as 24 minutes or more. You could think of this as an adaptive mechanism that makes up for the loss of restorative sleep. That is what forms the fundamental principle of all kinds of polyphasic sleep patterns. When the polyphasic sleepers deprive themselves of enough REM night after night from forceful awakenings, their brains delve into a rebound mechanism immediately after they go for a short nap in the next three or four days.
Can REM Rebound Hurt Your Health?
It is very common in patients undergoing CPAP titration. Untreated sleep apnea results in acute sleep deprivation. When people experience CPAP titration for the first time, they tend to enter a stage of a long REM rebound. Restorative sleep leads to heavy breathing and fast respiration rates. Therefore, people with severe obstructive sleep apnea (OSA) face a more significant threat from REM rebound than the general sleep-deprived populace. They are likely to enter deeper stages of restorative sleep, especially during the later portions of the titration. The type of architecture of restorative REM during the later phases of CPAP titration makes it more challenging for the OSA patients.
People do not wake up after each REM stage. However, cats and dogs do. In fact, almost all mammals, who live in the wild experience intermittent stages of wakefulness after each REM phase. These are the periods of “micro-awakenings” that intersperse sound sleep for most feline, canine and ungulate species. Research into their sleep behavior shows that it might be an adaptive mechanism that ensures the safety of their cohort while the other members sleep.
The windows of micro awakening help them survey their surroundings and weigh the threats from their predators before they nod off again. Depending on the extent of sleep animals require, an individual member can wake up from 6 to 8 times during their slumber.
Why do Some People Experience Disturbances during REM Sleep?
There are only a handful few in the world, who do not remember their dreams at all. Most of us remember them vividly and often recount the curious ones to our friends. Unless you cannot remember your dreams at all, you can be sure that you are getting REM sleep.
Nonetheless, there are a few unlucky ones, for whom rest is not just a cerebral experience. It is also a physical experience since they have to act it out during sleep. It is more common among children than it is among adults. Children often talk, move and walk in their sleep. Enacting dreams is not as odd for children as it is for the grownups. In a majority of the cases, these children grow out of this habit by the time they enter their teens or early twenties.
The problem of enacting dreams becomes dangerous when adults “pick it up” in their late teens or early twenties. Sometimes, people in their late 40s and mid-50s begin to move around, speak and walk in their sleep suddenly. These are telltale signs of REM-related sleeping disorders. Psychiatrists, psychologists, and sleep behaviorists refer to this as REM sleep-related behavior disorder (RBD).
The issues take a more severe turn when the RBD sufferers engage in physical harm, attacks or sexual acts in their sleep. Unattended cases of RBD have shown instances of adults unlocking their doors in the middle of the night or driving to a 24-hour store and wandering aimlessly on the streets. It is possible since these people do not undergo atonia and they can control limb movements during the REM stages.
When children go through night terrors, adults often try to calm them down by talking to them or shaking them awake. When adults experience such instances, it is more difficult to overpower them physically. Studies show that jostling sleepwalkers and RBD sufferers from deep sleep can harm them physically and mentally. Apart from removing sharp items, locking the windows securely, keeping the keys away and contacting a sleep expert, there is nothing much a concerned family member or friend can do.
Sleeping on the same bed with someone suffering from RBD is challenging and risky. The co-sleeper can experience physical injuries due to unpredictable movements. However, if you have a family member, who suffers from chronic RBD, you need to put your annoyance on the back seat and speak with a sleep expert for their proper treatment.
The cause of any REM behavior disorder can be complicated. Several interlaced factors can contribute to RBD, and those include genetic predisposition as well. Other factors include stress from daily routines, recent trauma, brain surgeries, brain tumors, depressive disorders, other psychosocial disorders and neurodegenerative disorders. Some medications like serotonin-modulating antidepressants, new opioid, and drug withdrawal therapy can induce RBD.
How do Experts Diagnose RBD in Individuals?
Studying REM is now simple with EOG and determining the presence of RBD in an individual is now equally quick with additional tests. The aim of most of these diagnostic tests is to study the physiological responses and signals of REM. Here are a few ways experts will determine if you or your loved one has RBD –
They will speak to you. There is no better way to find out if a person moves in their sleep than to ask their partner. If you move around, it is bound to wake your co-sleeper at one point or another. Once you and your partner can attest to the fact, experts can push further and recommend the diagnostics necessary for the process.
Thorough physical and neurological tests. A complete neurological test and physical exam will reveal if you have a predisposition towards RBD. It can also state if you have any other sleeping disorder that is masking itself in the form of RBD. In several cases, narcolepsy and sleep apnea show symptoms identical to RBD in adults.
Polysomnogram. Apart from electrooculography, doctors perform a polysomnogram on their patients to see how they sleep through the night. During polysomnograms, doctors may ask you to sleep over at a sleep clinic or lab. They will hook you up to monitors via sensors on your head, arm, legs, and chest. These leads will help them monitor your brain activity, limb movements, vocalizations, heart activity, and breathing.
Usually, multiple studies are necessary, since sleeping in a sterile environment like a sleeping lab is different from sleeping in a bedroom. If you have chronic breathing difficulties and REM awakenings in your bed, you might be suffering from severe allergic reactions unknowingly.
It is possible that you will sleep much better in a sterile environment than you would in your bed. Contrary to this, people have also reported feeling uncomfortable and sleep-deprived in clinics. Doctors sometimes make an exception and agree to set up monitors at home for critical cases.
What the Present Medical Treatments for REM Sleep-related Behavior Disorder?
Apart from physical safeguards, there are other pharmacological indications of RBD. Thankfully, the advancement of medicine has enabled people to experience a better quality of sleep irrespective of their REM challenges.
Melatonin: Melatonin is the human sleep neurohormone. Although human brains should produce this molecule naturally, not every person has enough supply of it. Therefore, doctors prescribe melatonin as a supplement. In several states, melatonin is an over the counter (OTC) product. You should be able to find OTC form of this naturally occurring hormone at any pharmacy. However, you should always consult an expert before beginning the dosage.
Clonazepam: Clonazepam has been one of the longest standing arch enemies of RBD. In fact, clonazepam and its other forms can combat any REM disorders in adults. It is not a medication for children. It is helpful for treating anxiety and chronic fatigue syndrome. However, it is not free from unpleasant side effects like worsening sleep apnea, decreased balance and coordination and daytime sleepiness.
While doctors keep investigating the other possible causes and treatments of REM sleep-related disorders, you should talk to your sleep specialist regularly. That will ensure that you are receiving the latest treatment and medication with the best possible benefits.
Before heading to a sleep clinic and spending a fortune on these fancy tests, you may want to consider the possibility of a false alarm. To rule out the possibility of a false positive, you can opt for smartphone applications, smart wearable technology, and headbands that can record your sleep duration, quality, and movements.
Millions of people around the world use these devices with sleep applications including white-noise generators and melatonin monitors to regain control over their sleep schedule. Always remember, these methods do not replace professional guidance and care. These are additional procedures that can give you the peace of mind before you step into a clinic worried about finding no treasure at the end of the hunt.
A Layman’s Take on REM and non-REM Sleep
You must have heard how your father could sleep through a blizzard and how your mother would wake up at the noise of leaves falling on the roof each night. While we were children, it was strange for us to believe that people could wake up to the sound of footsteps or falling leaves. For a few lucky ones, it is still unbelievable. However, most adults have faced the brunt of light sleep by now. It is a rough transition that finally lets us know that we have entered the adult stage of our lives.
Most babies and children sleep like a log. They can sleep through home reconstructions and the sound of jackhammers outside their window. Their blissful sleep is deep, and they spend most of their times dreaming. The incredible power of the child’s brain syncs the surrounding noise within the dream and allows them to stay relaxed even when there is possibly a parade outside.
It usually happens during the deep sleep or slow-wave sleep stages. It consists of the N3 and part of the N4 stages of non-REM sleep. It shows a lack of eye movement and the presence of muscle tone. It is an intrinsic part of memory formation in all ages.
These are the basic categorizations of deep sleep and light sleep most people experience. Light sleep is a form of non-REM sleep that makes up for 80% of an adult’s resting time. For children, REM sleep or deep sleep is much longer. Infants can sleep for about 16-hours per night, and they will be in the REM state for about 12 hours per day. Unless you baby has colic or some other physiological discomfort, he or she should sleep for 14 to 16 hours.
REM sleep is vital for their rapid growth, the formation of the cognitive and logical part of their brain, and proper rest. If you see your newborn waking up every 20 minutes to an hour, you must consult your pediatrician immediately. The same is valid for adults. Those, who do not experience enough delta sleep and REM sleep, experience impaired judgment, compromised cognitive abilities, and enhanced fatigue.
These are common effects of sleep apnea, sleep deprivation and shift-changing work that directly affect the sleep quality of individuals. The recurrence of REM and delta-sleep scarcity increases the chances of developing different types of cancer, Alzheimer’s, diabetes, heart problems and breathing problems.
Several studies have shown a direct link between the accumulations of beta-amyloid protein complexes (plaques) on the brain. These destroy the neuronal network and cause the deterioration of memory in adults. If a person’s genetics predisposes him to neurodegenerative diseases, the lack of enough deep restorative sleep can increase his chances of developing the disease in the future.
How to Gain Control over your REM Duration and Quality?
Unless you have been living under a rock for all these years, you must already know that the architecture of sleep is not as flat and dull as we surmise it to be. There are two primary stages – REM and NREM. These have sub-structures that include N1, N2, N3, and N4.
While N3 is a part of the deep sleep stage that involves delta wave activity or slow waves, N4 is the REM stage that helps with memory reconstruction. Rapid eye movement or REM sleep has a restorative function for the body and the brain. Therefore, it is only natural that people want to gain better control of the onset of it and its quality.
1. Exercise
It is no secret that the lifestyle we lead reflects directly on our sleep quality. The amount we work out each day and the kind of circuits we perform affects our sleep. Working out for about 20 to 40 minutes per day can help regulate your melatonin levels well, reduce the tendency to binge on sugary food and improve your body’s core temperature that can aid REM actively.
2. Regulating environmental temperature
While we are in the REM state, our core temperature falls significantly. We are unable to control it. It is easier to understand the sudden drop from the perspective of coldblooded creatures, which need an external source of energy to remain warm during the colder months.
Many RBD patients invest in smart sensors that determine the body temperature and adjust the temperature of the air conditioner to prevent rude awakenings. You can also time your AC to switch off at a particular time before it freezes your toes off. The reverse is advisable for people living in warmer climates.
3. Avoid certain food items
We all know about the eponymous enemies of sleep including sugary food and caffeine. The latest research shows that fatty food can take a toll on how you nap and rest throughout the night. Eating a bulk of deep fried and saucy food can keep you up for long, or it can force you to wake up repeatedly due to upheavals of your metabolism.
Caffeine stimulates wakefulness and Voltaire is known to have had 50-odd cups per day. Unless you are aiming at breaking his alleged record, you need to stay away from it post-evening. One or two cups of coffee are typical for the adults of the 21st century, but always have the last cup by 6 pm. Caffeine has a long half-life, and espresso at 8 pm can keep you up until 1 am.
4. Alcohol is not sleeping medication
There is no greater enemy of proper rest than alcohol. Thanks to Hollywood blockbusters and the glitz lifestyle, many US adults have the habit of going for a nightcap before they hit the hay. Our parents, grandparents and even their parents may have believed in the efficiency of a highball to knock us out like light, but they did not consider the after-effects of the delicious poison.
Apart from waking up to pee in the middle of a freezing night, the alcohol in the body can prevent your mind from entering REM altogether. Alcohol suppresses the release of the sleep hormones necessary for sound restorative sleep. You might find it easier to fall asleep initially after consuming enough liquor, but your chances of waking up after a couple of hours increase drastically.
5. Regulate your sleeping habit
What do you need more than diet and coffee every day? You need to regularize your resting schedule. Begin by going to sleep about 30 minutes earlier than usual. That will give you enough time to mull over the day’s happenings and recount the next day’s tasks.
Always let the thoughts flow freely before you float into a deep sleep. Having enough time to indulge in deliberate thoughts, imaginations and predictions will help you relax your mind. You will always know that you have time in hand for completing your rest and waking up on time for office. Unless you accommodate an extra half-an-hour into your sleeping routine, you will never learn the pleasures of true relaxation post-sleep.
6. Check your mattress
It might sound too trivial, but the quality of your mattress determines how well you rest each night. The number of allergens in your bedding, the hardness or softness of it and its age dictate the level of restoration. Mattresses tend to lose their support over the years. Some of them require replacement after 6 to 8 years.
Check the manufacturing date of yours to find out if it is still usable. Children grow up faster, and they need sound sleep. Therefore, their mattresses require regular cleanup, maintenance, and replacement. Super hard or excessively soft bedding can hinder REM by causing sharp pains and discomfort. If that is the case with you, you should try memory foam or orthopedic mattresses to assist better sleep.
No matter how acute your problem is and how efficient you are in self-diagnosis, it is never advisable to try OTC treatments for sleep apnea or RBD. All forms of sleep deprivation require medical attention. Chamomile tea, jasmine infusions, aromatherapy and relaxing spas can help you find some relief from the stress and fatigue building up over the days.
In most cases, these methods of ineffective in inducing or improving REM sleep in patients. In short, there is no cheaper or easier replacement for expert diagnostics and care for REM sleep disorders. If you think you might have one, you can begin by installing sleep monitor applications or buying pocket-friendly wearable technology. However, always know that sleep experts and medical experts should oversee the final treatment.