Category: news
A new study looks into the relationship between sleep duration, mental health, cognitive performance, and brain structures in children.
Childhood is a crucial period for the development of our central nervous systems, making it imperative that during this time, children are provided with all necessary essentials. This encompasses appropriate nutrition, both physical and mental stimulation, a sense of joy, and, importantly, sufficient sleep.
Sleep is essential for proper cognitive functioning. It is well known that lower sleep duration is correlated with cognitive and mental health problems in adults. However, a large scale analysis of this correlation has lacked in children.
A new 2020 study wanted to analyze the impact of sleep duration on psychiatric and cognitive problems, and also see how it impacts different brain structures.
Researchers from the University of Warwick investigated over 11,000 children aged 9-11 from the Adolescent Brain Cognitive Development (ABCD) consortium. All the children came from the US with a wide range of geographic, ethnic, socioeconomic, and health backgrounds.
Behavioral measurements were used to obtain sleep duration, cognitive, and mental health assessments. Researchers also looked at structural MRIs to see if there were any changes in central nervous system composition in relation to sleep duration.
After statistical analyses, researchers found that the feelings of anxiety, depression, and impulsive behavior were negatively correlated with the sleep duration in participants. The same could be said with cognitive performance. Interestingly, the mental well being of parents was also negatively correlated with the amount of sleep their children were getting.
Looking at the neural imaging, researchers noticed a trend of lower brain volumes, especially in particular areas such as temporal, prefrontal, and orbitofrontal cortex, inferior and middle temporal gyrus, precuneus, and supramarginal gyrus.
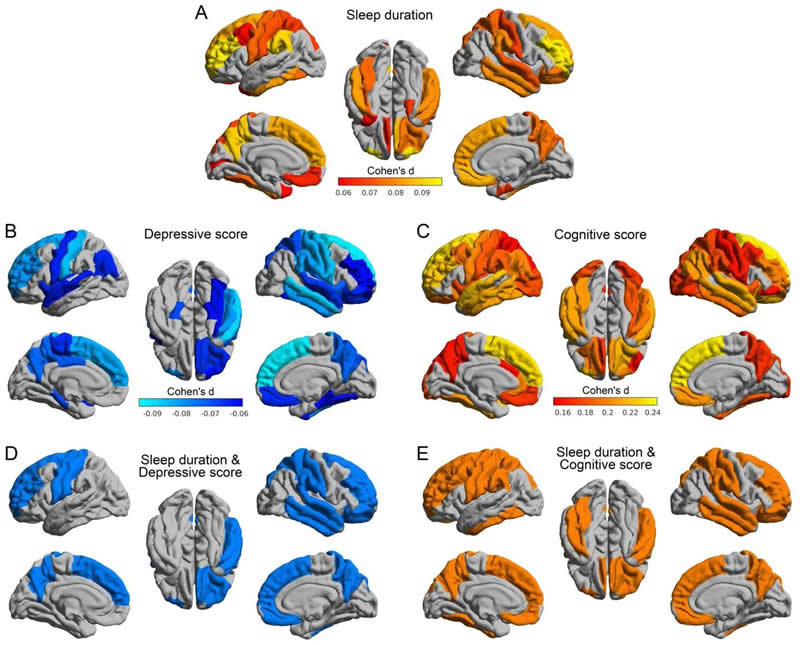
Different brain areas affected by sleep. Source: University of Warwick.
After one year, a follow up with around half the initial participants showed depressive symptoms were correlated with shorter sleep duration even at that time. Since there is a complex link between sleep and mental health, we often see sleep disturbances in people with depression and anxiety. And it can be hard to break from that circle since mental health problems make it harder to maintain good sleep hygiene, and a lack of proper rest makes these conditions worse.
The biggest problem is that the majority of children don’t get enough sleep on school nights. Inappropriate screen time, the use of electronics before bedtime, inadequate school schedule, too much homework, and other activities can all impact your child’s rest. However, you should try your best to teach them the importance of sleep.
One of the coauthors, professor Edmund Rolls stated that children who slept for less than 7 hours on average expressed 53% more behavioral problems and had a 7.8% lower cognitive score than children who slept 9 to 11 hours. These numbers should highlight just how essential sleep is for both mental health and cognitive performance.
Although we need that sleep is vital, especially in the developing period, researchers admit that we need more studies to discover the underlying mechanisms for these links.
A new study shows that odor cues such as rose scent during learning and sleep improve vocabulary learning and test performance in 6th-grade students.
For many, the idea of acquiring knowledge while asleep has long been an enticing concept. However, attempts by some to master languages like Spanish or Chinese by playing lessons as they slept soon revealed that this technique wasn’t particularly effective. While sleep plays a crucial role in learning, it cannot substitute for the effort required to learn.
However, a new study from the University of Freiburg shows it could be possible to optimize sleep and achieve more efficient learning.
The team of researchers wanted to assess the importance of odor cues during learning, sleep, and testing, on memory formation in school children. Some previous studies performed in laboratory conditions showed that odors could be a potent stimulus for memory consolidation during sleep. However, this new study wanted to explore how this hypothesis would hold in everyday conditions.
The study was conducted in 6th-grade healthy German students in their home and school environment. To see how odor impacts learning English vocabulary, researchers used rose scent as an odor cue. They divided the students into four groups
- The control group didn’t receive any intervention.
- The second group had a rose scent present while they were studying and sleeping.
- The third group had a rose scent present while learning and taking a test.
- The final group had a rose scent present while learning, sleeping, and taking a test.
The results surprisingly showed that the students remembered vocabulary much better with a rose scent. In fact, the students who were exposed to rose scent during learning and sleep showed a 30% increase in learning success compared to the control group. There was no difference between the second group where the fragrance wasn’t present during testing and the last group where it was present during all three phases. The researchers published these findings in the Nature Group’s Open Access journal Scientific Reports.
These findings suggest that a simple fragrance stick could be used for improving learning efficiency. It highlights the importance of odor cues in memory acquisition and consolidation. And if something so simple could be this efficient, everybody could boost their learning ability with ease.

However, there are a few limitations to this study. The participating students went to two different schools, meaning different teachers, classes, and tests. That could very well be a reason for some of the result differences. Also, there was no control over other environmental factors. Students were responsible for studying, and the use of scented sticks and their reports may not reflect these parameters objectively. That is why scientists perform these experiments in a lab, where they can control all the factors, but this study provides valuable insights nevertheless.
This could be a significant step towards making learning more efficient and improving the effect of sleep on memory formation.
A new study from the Uppsala University shows how a single night of sleep could increase blood levels of a recognised biomarker of Alzheimer’s disease.
Every expert sings the same tune: skimping on sleep spells trouble for your well-being. Whether it’s the quick hits of feeling grumpy, worn out, and not on your A-game, or the big-time risks of long-term snooze shortages.
However, a night or two of poor sleep shouldn’t have long term consequences. The following day may be harder to manage, but once the regular sleep schedule is back, everything turns normal. We’ve all been there, whether we had to pull an all-nighter, experienced jet lag, or were stressed or excited so much that we couldn’t sleep.
But, a new study from Uppsala University published in the medical journal Neurology hints that even a single night could have serious consequences, like an increase in a common biomarker of Alzheimer’s disease.
Participants were 15 healthy young male adults with an average age of 22 years and a healthy BMI index. They all stayed in a lab, had the same activity and meal patterns, and they also experienced two types of interventions at random. They either had a night of normal sleep, or they had to stay up and experience sleep deprivation. To stay awake, they were permitted to watch movies, play board games, and they were engaged in a conversation with experiment leaders to ensure wakefulness.
After each night, researchers took their blood samples and tasted it for several different markers of central nervous system health. Researchers looked at beta-amyloid, tau proteins, as well as levels of other factors that are commonly linked with neurological disorders.
This preliminary study found that acute sleep loss led to a 17.2% increase in tau protein blood levels. This molecule is located in the neurons of patients with Alzheimer’s disease, and it can start to accumulate decades before the symptoms appear. That is why finding the cause behind this increase in tau protein levels could help manage Alzheimer’s.

There were no changes in other biomarkers of cognitive health.
And while researchers state that the increase of tau blood level is not a good thing, it doesn’t have to be necessarily bad. Higher activity of neurons during wakefulness could lead to a higher synthesis of this protein, and it’s higher blood levels could simply reflect the overall increase. More tau in blood could be a direct consequence of the brain trying to clear itself.
A few limitations, like small sample size, were reported. Also, the subjects were all young, healthy males, and the results could be different in other groups. It is particularly interesting to see how things would play out in older individuals since they have an increased risk of dementia and different lifestyle habits.
However, the study could provide a valuable inside into an early onset of dementia and Alzheimer’s disease. It could help us understand how sleep impacts these conditions and possibly set new guidelines for lowering the risk of developing them.
A new study suggest that weight lost leads to upper airway changes such as reduced tongue fat, which could improve obstructive sleep apnea symptoms.
Obstructive sleep apnea (OSA) is a significant disorder related to sleep that impacts over 22 million people in the United States. Individuals suffering from this disorder experience several interruptions in their breathing while asleep, significantly affecting their sleep quality. Snoring is the most frequent sign of this condition, and individuals often suffer from excessive tiredness during the day. It’s critical to take this condition seriously as it may result in higher blood pressure, cardiovascular issues, and strokes.
It has been known that obesity is one of the main risk factors for developing sleep apnea, and when you consider that more than 70% of adults in the US are overweight, the situation is alarming. Standard treatment options for sleep apnea include continuous positive air pressure (CPAP) treatment and weight loss. However, CPAP is not always effective, and weight loss only seems to work in some instances.
That is why scientists from the University of Pennsylvania’s School of Medicine looked into the mechanisms in which weight loss improved sleep apnea symptoms.
Their 2019 study used magnetic resonance imaging of upper airways to measure the effects of weight loss on OSA symptoms. They found out that weight loss leads to reduced tongue fat, which was the strongest impact on decreasing the severity of OSA.
The findings were published in the American Journal of Respiratory and Critical Care Medicine, and their results could have a significant impact on future treatment of sleep apnea. Since we now know what the primary reason for airway obstruction is, we can find ways to target it and lose tongue fat more efficiently.
One of the co-authors MD Richard Shwab led a previous study where he compared obese people with and without OSA. He already determined that patients who had OSA also had significantly larger tongues. The next logical step would be to assess how reducing tongue fat would affect OSA symptoms, which is precisely what this new study does.
The study included 67 obese participants with mild to severe sleep apnea. During a six month intervention, participants underwent diet adjustment or weight loss surgery which resulted in a 10% bodyweight reduction on average. Sleep study after the weight loss intervention showed that patients’ sleep apnea score improved by 31%.
And with MRI scans, researchers were able to locate the exact upper airway changes that led to this decrease of OSA symptoms. Tongue fat loss was the number one predictor of improvement, but also loss of soft tissue, reduced jaw muscles, as well as decreased muscle size on the sides of the airway all improved sleep apnea.

These findings could help us create an effective way of reducing tongue fat either through surgical procedures or possibly special diets that target fat loss in this area. These interventions are yet to be tested.
Shwab’s team is also interested in whether people who aren’t overweight but have fatty tongues could be predisposed to developing OSA. They think that because they have an average body mass index, they are less likely to get the right diagnosis, which poses a threat to their health. Their future research should shed some more light on this issue and help us get the most effective sleep apnea treatment.
Scientists have identified miRNA molecules that correlate with sleep duration in children and adolescents. Possible blood tests for assessing sleep hygiene.
Considering that sleep plays a crucial role in the growth and development of children, numerous individuals are concerned that their children are not receiving adequate rest. Lack of sufficient sleep may result in various health issues, such as diabetes, elevated blood pressure, and a higher risk of numerous diseases. While monitoring sleep can provide a reasonable assessment of their sleep quality, it is significantly subjective and not completely dependable.
But now, it seems like scientists have found a way of assessing sleep hygiene in children with a simple blood test.
A new study published in the journal of Experimental Psychology by the Physiological Society looked into certain markers in blood and how they correlated with sleep duration in children and adolescents.
A team of Italian researchers investigated 111 normal-weight children based on their body mass index. All participants came from eight European countries, including Italy, Spain, Germany, Belgium, Cyprus, Sweden, Estonia, and Hungary, and they were divided into two groups based on their self reported sleep habits.
The short sleeping group included children and adolescents who slept less than their minimal daily recommendation, which is 9 hours for children under 13 years and 8 for teenagers. The normal sleeping group consisted of children and adolescents who met their daily minimum sleep requirements.
Then scientists analyzed micro RNA (miRNA) blood levels. These molecules, among other functions, serve an essential purpose of carrying information about which genes to turn on and off. Since they regulate the activity of our genome, scientists wanted to see how they affected sleep during a young age.
They found the concentrations of two miRNA molecules to be different in normal and short sleepers. Even when they took into account participants’ age, sex, pubertal status, country of origin, screen time, and parents’ education levels, it didn’t change the outcome of the results.
These results could help us create a blood test that would detect these molecules, and objectively asses sleep hygiene in children and adolescents. That could also be useful in preventing many health impairments due to lack of sleep. This objective measurement could prove to be a helpful tool, as relying on self-reporting questionnaires depend on our subjective view.

However, the authors reported a few limitations of their study, such as a weak correlation of sleep duration and miRNA blood levels in the normal sleeping group, and no significant association in short sleepers. Additionally, self-reported questionnaires could be inaccurate, although they are commonly used in sleep assessment studies. Researchers also didn’t include physical activity in the analysis, and this variable could be crucial.
Generally, sleep duration and quality are affected by many different factors, such as genetics, environment, and others. These findings concerning miRNA concentrations and sleep duration during a young age, even though still weak, could prove to be vital for further research. Of course, more studies are needed to explore the function and importance of these miRNA molecules.
A new study from Hokkaido University shows the role of MCH neuron activity during REM sleep in forgetting new information and maintaining brain plasticity.
The text you’ve provided for rephrasing appears to be missing, as the content you’ve indicated ( ) translates into a non-breaking space in HTML, used to create a space in webpage coding. There’s no actual text or sentence provided for rephrasing. Could you please provide the specific text or sentence you need rephrased?
The link between sleep, memory, and learning has been puzzling scientists for decades. It is clear that the memory forming process is closely related to sleep, and you wouldn’t be able to learn anything without it. But the mechanism behind how it all works is still a great mystery.
A new study from Hokkaido University in Sapporo, Japan, indicates that REM sleep is not only essential for learning, but it could be responsible for our ability to actively forget. It appears that forgetting things isn’t a random process at all, and neurons control it via certain hormones.
We are bombarded with millions of stimuli and new information every day. It would be impossible to remember all of this, which is why your brain must learn to recognize what’s essential and what’s not. Unimportant stuff gets discarded, and our brains don’t get overloaded. And it all happens during REM sleep.
Rapid eye movement or REM sleep is a sleep stage when most dreams occur, especially vivid ones. Scientists have long hypothesized that dreaming is important for memory by sending signals through specific pathways and strengthening neural circuits. But now, this new study on mice indicates that REM sleep could be the time when our brain decides what is not important, and activates mechanisms to forget that information actively.
Some scientists like Francis Crick – the co-discoverer of double-helix DNA structure, have hypothesized about the role of sleep, especially REM phase, in our ability to get rid of the excess information. But before this study, we had no idea about the mechanism of how the brain prunes certain synapses involved in learning.
A team of Japanese and US researchers was particularly interested in neurons producing melanin-concentrating hormone (MCH), which is known to play a role in the control of appetite and sleep. It turns out that the majority of MCH neurons (52.8%) in the hypothalamus are active during REM sleep. Around 35% fire during waking hours, while 12% are active during both states. And it seems that these MCH cells send inhibitory signals to specific memory centers like the hippocampus.
To test the effects of MCH cell activity, researchers used different genetic tools to turn them on or off and see what kind of impact it would have on memory. They were particularly interested in the retention of new information before it had the time to be incorporated into long-term storage.
And the results surprised them, as turning on MCH neurons had a negative impact on memory retention, and mice performed worse on memory tests. On the other hand, when MCH neurons were shot down, memory test results improved. That was only effective when managing MCH neurons during REM sleep. Turning them on and off when awake or during other sleep stages had no impact on memory retention. One of the authors, Dr. Kilduff, explained this by hinting that the activation of MCH cells could be to prevent the content of dreams from storing into long term memory.
Researchers plan to investigate how these new findings could help us learn more about memory-related conditions such as Alzheimer’s, as well as sleep disorders. One thing is sure; sleep remains one of the essentials for a good memory!
Research has shown that cognitive behavioral therapy is an effective way of fighting the symptoms of insomnia. Learn how CBT can help you if you are struggling with insomnia.
In today’s fast-paced society, our lifestyles have undergone significant transformation. We find ourselves constantly on the move, buried in work, and overwhelmed by stress from numerous sources. This includes exposure to screens that produce blue light, disrupting our body’s natural rhythm, as well as the sounds permeating from city surroundings.
As a result, our sleep is often suffering. It is no wonder that we have a pandemic of sleep disorders. One of the most common sleep disorders is insomnia, and it is estimated to affect around 30% of people at some point in their lives.
Treating insomnia is a challenging task, and it can be different depending on the individual. Cognitive behavioral therapy (CBT) is the first option for treating insomnia. It is supposed to be a long-lasting solution, in contrast to medication that is used to help manage short-term symptoms of insomnia.
Research done so far has shown that CBT is an effective way of lessening and eliminating symptoms of insomnia. Let’s dig in into different aspects of CBT, how it works, what are the benefits, and why you should try CBT if you are struggling with insomnia.
What Is Insomnia?
Insomnia is one of the most common sleep disorders, where an affected person is either not able to fall or stay asleep. Depending on that, a person is diagnosed with either sleep onset or sleep maintenance insomnia.
Everyone experience a sleepless night now and then, and if it just one night, you probably shouldn’t worry about it. Maybe you had an afternoon nap, or you got too excited about some event, and your nightly rest suffered a little bit.
If the symptoms persist for some time, it is probably best to seek professional medical help. Some people may experience a condition called transient insomnia, which can last up to three months. It can usually be connected to a stressful period, some acute illness, hospitalization, or a significant life event. It can even be caused by a rebound effect when a person stops using sleep medication. The important thing is that the situation usually resolves when the conditions go back to normal.
Chronic insomnia is a little different. Environmental factors can trigger it, but genetic factors and underlying conditions play a significant role as well.
Some people have a naturally low threshold for nighttime arousals, which is why their sleep is often fragmented, and they are more prone to developing insomnia. Others might have a condition like restless legs syndrome, chronic pain, depression, anxiety, kidney disease, arthritis, Alzheimer’s, or some other medical condition that is affecting their sleep.
If that is the case, besides standard insomnia treatment, doctors also focus on eliminating the underlying causes and managing the disease that is responsible for sleep disruption.
What Is Cognitive Behavioral Therapy for Insomnia (CBT-I)?
CBT-I is a go-to treatment when it comes to insomnia. It consists of a series of visits to a psychologist who specializes in this type of treatment. The goal of CBT-I is to address problems surrounding sleep and to create a more peaceful sleep environment, as well as a positive attitude towards your nightly rest.
CBT-I is used for treating chronic insomnia since people usually develop negative thoughts and behaviors connected to their sleep. It is understandable that after tossing and turning in bed for a long time, people tend to get a bit frustrated. And if this persists for weeks or months, you might go to bed every night expecting to get inadequate rest.
That is where CBT-I steps in and tries to turn these negative associations into positive ones. That takes time, and CBT-I is often viewed as a long term solution for sleep problems. Standard CBT-I program involves regular sessions for 6 to 12 weeks, and it includes different approaches based on each case.
The CBT-I can include stimulus control, sleep restriction, biofeedback, relaxation training, and sleep hygiene education. The treatment usually consists of a combination of these approaches, and sometimes you can even be prescribed medication for short term relief if the symptoms are severe. It is all closely watched by a sleep specialist, who evaluates your condition with each weekly session, and they adjust the treatment accordingly.
Stimulus Control
People with insomnia often have a lot of negative thoughts about sleep. They get frustrated with the inability to fall asleep, which can later develop into anxiety. That results in a negative attitude towards going to sleep, as people are already expecting a negative outcome.
Stimulus control aims to reinforce positive associations with sleep and to get rid of any distracting thoughts. That usually means using your bed only for nightly rest and intimacy and leaving all electronics, and other distractions from your bedroom. All other activities like watching TV, reading, catching up with news, or looking up social networks should be left outside the bedroom.
When you get rid of distractions, it should be easier to fall asleep. However, if you have been in your bed for 20 minutes, and you haven’t fallen asleep, it is time to get up. Doing some relaxing activity should wear you out, and then you can return to bed when you feel tired again.
After some time, your brain learns to recognize the bedroom as a place for relaxation, and nightly rest. That means that it takes less time for you to fall asleep, and all the negative thoughts surrounding sleep will slowly go away.
Sleep Restriction
Most people think that going earlier to bed should result in more sleep. However, that is not true in most cases, since more time in bed doesn’t necessarily mean more rest. Our internal clocks dictate our sleep and wake cycles, and the best thing you can do for your internal clock is consistency. Going and getting out of bed at the same time every day is one of the most important things when it comes to good sleeping habits.
Sleep restriction limits the time spent in bed each night in an attempt to cut down the time needed to fall asleep. For instance, if you usually spend 7 hours in bed each night, but you only get 4 hours of sleep, the initial limit is set at 4 hours.
Sleep restriction seems to have an opposite of the desired effect in the beginning, since you are spending less time in bed, you are not getting enough sleep. But with time, falling asleep becomes more comfortable, and your sleep efficiency increases. After that, you start gradually increasing your time spent in bed until you can regularly get sufficient amount of sleep without prolonged sleep onset and nocturnal disturbances.
Biofeedback and Relaxation Techniques
These two usually go hand in hand as the ultimate goal is for you to calm down, and enter a relaxed state that should make it easier to fall asleep.
Biofeedback refers to using a small device that tells you about the state of your body. This device tracks your heart rate, blood pressure, muscle tension, or body temperature, and can tell you when these parameters change. The device alerts you when these parameters increase, which is an indicator that you are getting restless. Using these devices comes naturally for some people, while others need time to get used to them. Either way, don’t worry and take your time.
After you learn to recognize the signs of restlessness, it is essential to know how to reverse your mind and body into a calm state. That is when relaxation techniques come into play, and the most common ones include meditation and breathing exercises.
With biofeedback and relaxation techniques, you will learn to recognize when you are getting frustrated with the inability to fall asleep, and also to calm yourself. That is useful not just for sleep, but for other aspects of your life as well.
Sleep Hygiene Education
One of the first things a sleep specialist does is examining your lifestyle habits. People often do certain things that disrupt their nightly rest, without them even realizing. That is why it is crucial to learn about good sleep hygiene and make some adjustments to help you sleep better. That includes:
- Sticking to a regular sleeping schedule. Going to sleep and waking up at the same time every day helps your internal clock realize when is the time to be active, and when you should go to sleep. Staying up late and sleeping in on weekends is tempting, but you should avoid it and stick to your schedule.
- Making your bedroom sleep-friendly. You should remove all the distractions from your bedroom, including all electronics and anything that can wake you up. Keep your sleep environment dark, and set the room temperature to mid 60 Fahrenheit, as it appears to be the best sleeping temperature.
- Avoid screen time at least 45 minutes before bedtime. Screens emit blue light that can make your brain think that it is daytime, and it stops the production of melatonin. Melatonin is a sleep-inducing hormone that is produced at night, and it is vital for our sleep/wake cycles. If your brain stops producing melatonin before bedtime, it becomes more difficult to fall asleep.
- Create a relaxing bedtime routine. You can try reading, taking a hot bath, listening to relaxing music, yoga, meditation, breathing exercises, or tending to a hobby. Just remember to do it outside the bedroom, as the bed should be reserved only for sleep related activities.
- Eat a balanced diet, with a lot of fruit and vegetables. You should also stay away from stimulants like nicotine, alcohol, and caffeine at least 6 hours before going to bed, as they can disrupt your sleep.
- Exercise regularly. Staying active is essential to proper rest, and experts recommend at least 150 minutes of moderate activity each week for full long term health benefits. However, don’t exercise too close to bedtime, as it can be counterproductive and make it harder to fall asleep. You should also spend some time outdoors in daylight each day, to help your biological clock understand when active hours are happening.
On top of all of these techniques and education, a sleep specialist will discuss everything with you during weekly sessions. They can discover underlying sleep problems, tell you where you go wrong and point you in the right direction. Even though it may seem like all of these different techniques aren’t complicated, having a professional guide you makes it much easier.
Is CBT-I Effective?
It all means nothing if CBT is not effective for treating insomnia. Luckily, there has been a lot of research, where scientists investigated aspects of CBT and how it compared to sleep medication.
This 2002 meta-analysis tried to discover how effective sleep medication and behavioral therapy were in treating chronic insomnia. The review looked at different parameters, including total sleep time, sleep latency, number of nighttime arousals, wake time after sleep onset, and sleep quality. All of these were assessed before and after the treatment was conducted. The results showed that both pharmacotherapy and behavioral therapy are an effective way of treating short term effects of primary insomnia. There was no difference in effectiveness between those two, except in sleep latency, where CBT showed a more significant reduction in sleep latency.
A 2004 study looked at different treatment approaches for insomnia. The results showed that CBT was the most effective intervention, and it also produced the most persistent improvement in sleepers. That was another step in proving the effectiveness of CBT, and placing is as the number one treatment for insomnia.
The results of later research followed the same trend. This meta-analysis also highlighted that CBT-I is at least as effective as pharmacotherapy in the short term, and it is superior in the long term. Because of the long-lasting effects of CBT-I, it is considered a first-line treatment for insomnia.
Besides insomnia, CBT has been proven effective for some other conditions, like anxiety, depression, and chronic pain. A 2012 study showed some long term effects of CBT on patients with chronic pain. There was a 23-minute improvement in total sleep time recorded six months after the treatment. That showed that CBT was valid and that it also had long-lasting effects.
When to See a Professional
If you occasionally experience a night of poor sleep, there is probably nothing to worry about. However, if your problems persist for some time, you might need to see a professional. If your everyday life and work performance are affected, it is time to book an appointment.
Medical professionals will help discover the cause of your sleep problems, and prescribe you the needed therapy. Depending on what’s causing your sleep problem, it could even be CBT.
If you have been advised to try CBT-I, it is vital to remember that it has been proven effective time after time. Stick to it even though it might not seem like it’s working in the beginning, it will definitely pay off in the long run.
Did you know that keeping certain houseplants can ensure you catch those precious ZZZs? Houseplants aid sleep by improving air quality, raising the oxygen levels in the room and emitting moisture to combat sinus issues and ensure easier breathing while you snooze. Here are our top 8 plants for the bedroom to help you sleep like a baby.
Need some extra help in the sleep department? Some folks have a very easy time falling asleep naturally, but for others, it can be a real hassle. If you didn’t get a full 8 hours of blissful, uninterrupted sleep last night, don’t immediately reach for herbal supplements and melatonin pills – consider upping your home flora game instead!
You probably know that certain herbs such as chamomile and lavender can help you sleep better when you consume them, but did you know that keeping certain houseplants can also ensure you catch those precious ZZZs? Houseplants aid sleep by improving air quality, raising the oxygen levels in the room and emitting moisture to combat sinus issues and ensure easier breathing while you snooze. Here are our top 8 plants for the bedroom to help you sleep like a baby.
How Houseplants Aid Sleep?
Houseplants are mostly known for their ability to purify the air and help you breathe better. However, some plants, apart from their air-cleaning properties, also come with other relaxing traits, that can be really useful for getting a more peaceful and healthier snooze.[1] The interesting part is that each plant helps in different ways. For example, some plants such as Aloe Vera and Spider plants, release a lot of oxygen and absorb the carbon dioxide we exhale during the day which is great for purifying the air and helping you breathe more comfortable in the evening.[2]
Houseplants are also very good at absorbing common VOCs (volatile organic compounds) such as trichloroethylene, benzene, formaldehyde, xylene, and ammonia. Let’s take a quick look where can these VOCs be found.
- Trichloroethylene – an industrial product found in paints, dry cleaning, and adhesives.
- Benzene – a common solvent found in gasoline, oils, rubbers, and plastics.
- Formaldehyde – a water-soluble organic compound found in grocery bags, cleaning agents, and paper towels.
- Xylene – a chemical found in tobacco smoke, rubber, paint, and vehicle exhaust.
- Ammonia – commonly found in household cleaners, floor wax, and fertilizers.
Other plants, such as lavender, jasmine, and gardenia, apart from purifying the air and absorbing VOCs, release relaxing aromas that particularly help with reducing anxiety, relieving stress and helping you get a more peaceful night’s rest. To enjoy the healing and relaxing aromas of different herbs, you don’t need to diffuse essential oils or create incense – housing live plants in your bedroom is enough.
Sounds too easy or too good to be true? As always, Counting Sheep backs up everything with science! One of the first studies that examined the benefits of houseplants was done in 1989 by NASA, and the research was focused on finding out how some houseplants purify indoor air.[3]
In the Journal of Physiological Anthropology, researchers have found out that the plant known as vining pepper improves workers’ moods when introduced to a work environment. The study suggests that indoor houseplants can reduce physiological and psychological stress, and evoke calmness.[4]
Lastly, another study showed that flowering and foliage plants improve the health of recovering surgical patients, especially when it comes to reducing their fatigue and anxiety levels.[5] According to the results of the study, indoor plants may decrease the patients’ needs for medicines, help them cope better with stress and pain, and promote positive physiological responses, as well as more positive feelings.
Now let’s take a look at the top 8 best plants for sleep.
Aloe Vera – Best Plant for Improving Air Quality
Listed as one of NASA’s top air-improving plants, the fantastic Aloe Vera aids sleep by emitting oxygen at night, ensuring you are breathing easier and making you more room for a peaceful slumber. It’s also great for purifying VOCs such as benzene and formaldehyde.
When it comes to maintenance, it’s very easy to grow and tolerates neglect well. It doesn’t need a lot of direct sunlight and frequent watering, so it’s perfect if you are a student, employed, or simply someone who doesn’t have much free time.
Known in Egypt as the plant of immortality, it reproduces quickly and easily, meaning that if you buy one, you can easily have an Aloe for all the rooms in the house. Apart from helping you sleep better, you can use the gel from its leaves to treat minor cuts or burns, insect bites, and much more. Considering all its benefits, it’s a must-have plant in every home.
Jasmine – Best Plant for Relaxation
Jasmine flowers are known for their sweet smell, that is often found in perfumes, candles, shower gels, hydrating milk and so on. The pleasant aroma of this exotic plant has a calming effect on the body and mind. Studies show that it reduces anxiety, helping you to cope better with stress or anxiety-related insomnia.[6]
Jasmine is an effective sleep aid specifically because of its sweet fragrance, and multiple studies have found that sleeping in a room with this plant improves sleep quality.[7] To take proper care of your Jasmin plants, ensure they get direct sunlight during summer and spring. During winter avoid direct sunlight. Watering is very simple – just make sure the soil remains moist.
Lavender – Best Plant for Deeper Sleep
Who doesn’t love the scent of lavender? Lavender is definitely one of the most well-known plants that induce sleep and reduces anxiety and stress levels.[8] Research shows that lavender scent slows down your heart rate, and lowers your blood pressure, making you feel more relaxed and calm.[9]
According to a 2013 study in the journal Evidence-Based Complementary and Alternative Medicine, lavender aromatherapy improved the sleep quality in multiple study participants among which were healthy students, ischemic heart disease patients, and women suffering from insomnia. Also, taking lavender oil orally at the dose of 80mg per day increased the quality and duration of sleep among patients who struggled with mixed anxiety disorder.[10]
Lastly, one study shows that the smell of lavender is so pleasant that it even calmed down crying babies[11] and sent them into deeper sleep – this is something definitely all new mothers will be glad to hear!
While there is a host of lavender scented products on the market that can help you get a good night’s rest, why wouldn’t you simply go for the most natural and cost-effective option, and that’s to place a beautiful lavender plant right on your nightstand.
Snake Plant – Best Plant for Air Purification
Snake plant, similar to Aloe is considered one of the best houseplants for improving indoor air quality. Japanese researchers that have published their study in the Journal for the Food and Agriculture Organization of the UN found that this plant absorbs various hazardous chemicals, leaving indoor spaces safer and a lot cleaner. The Snake plant is best for filtering nasty household toxins such as formaldehyde, trichloroethylene and benzene from the air.
Gardenias – Best Plant for Relieving Anxiety
Gardenias have glossy green leaves and beautifully scented blossoms, which makes them a very popular plant choice for bedrooms. Studies show that keeping this houseplant in your bedroom improves air quality, promotes better sleep and relieves anxiety. Particularly, the results show that one of the carotenoids found in Gardenia, called Crocetin, improved sleep quality in men who suffered from problems associated with sleep, with no additional side effects.[12]
The only downside is that gardenias can be a bit difficult to maintain. In order to keep their delicate leaves and flowers, you have to keep it on bright, but indirect sunlight, and regularly spray its leaves and soil with water. If you suffer from insomnia or anxiety, investing a bit of your time of taking care of this plant could be a much better and healthier solution to taking sleep pills.
Spider Plant – Best Plant for Filtering VOCs
Spider plant, similar to snake plant is also considered one of the best houseplants for filtering VOCs, and its air-cleaning properties and health benefits have been scientifically confirmed. According to NASA tests, spider plant has the ability to remove 90% of chemicals like benzene, formaldehyde, carbon monoxide, and xylene from the air.[13] Since formaldehyde is found in many common household products, it’s a good idea to keep one of these plants around. Apart from cleaning the air and improving the oxygen levels in your bedroom, this plant is also great for absorbing fumes and odors.
Spider plants are very easy to maintain, making them perfect for busy owners who don’t have time to provide constant care. The only thing this houseplant needs is well-drained soil and indirect light. Spider plants don’t like to be overwatered and prefer cooler temperatures (anywhere from 55 to 65 F).
Valerian – Best Plant for Inducing Sleep
The Valerian is a flowering plant known for its beautifully scented pink or white flowers that bloom in the summer. The plant doesn’t take much space, and its long stalks and colorful flowers will be a wonderful addition to any bedroom.
The blossoms are used as a perfume since the 16th century, while the root has been used for tea or tincture since ancient times. It’s an interesting fact that a Roman physician and philosopher named Galen prescribed Valerian for insomnia. Today, research has proven that Galen was right and that valerian root can indeed alleviate sleep issues.[14] When it comes to this plant’s sleep-inducing properties, the effect comes from a number of chemicals, specifically isovaleric acid and valepotriates that help to relax the muscles and the central nervous system.[15]
Valerian is so powerful that inhaling its scent is enough for falling asleep faster and enjoying a more peaceful night’s rest.
To take proper care of your Valerian, make sure it receives a lot of sunlight and water it enough to keep the soil moist.
Peace Lily – Best Plant for Increasing Humidity
Apart from looking exceptional and being amazing air cleaners,[16] Peace lilies can also increase room humidity by up to 5%. Increased humidity is not only great for easier breathing during sleep, but also for getting rid of any impurities and airborne microbes that could disturb your rest. Studies show that sleeping with peace lilies helps to decrease one’s susceptibility to colds and respiratory illness.[17]
To take proper care of this plant, keep it in a shady spot and water it once a week, best when top inches of the soil seems dry.
The Bottom Line
And that’s it! According to our research, those were the 8 best plants for sleep!
Among some of our honorable mentions are English Ivy, Pothos, Passion Flower, Bamboo Palm, Chinese Evergreen, and Dracaena.
As you can see, there definitely isn’t a lack of houseplants that can be used to aid you in your sleep. They add warmth, relaxing fragrance and effectively increase oxygen levels in your room, thus ensuring a restful slumber. Add one of them in your bedroom to get your own little dose of zen.
Resources and References
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3230460/
[2] https://www.researchgate.net/publication/319979551_Role_of_Plants_in_Indoor_Air_Remediation
[3] https://ntrs.nasa.gov/archive/nasa/casi.ntrs.nasa.gov/19930073077.pdf
[4] https://jphysiolanthropol.biomedcentral.com/articles/10.1186/s40101-015-0060-8
[5] https://journals.ashs.org/horttech/view/journals/horttech/18/4/article-p563.xml
[6] http://article.sapub.org/10.5923.j.health.20170704.01.html
[7] https://www.sciencedaily.com/releases/2010/07/100708104320.htm
[8] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6007527/
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3612440/
[10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5878871/
[11] https://www.ncbi.nlm.nih.gov/pubmed/18053656
[12] https://www.ncbi.nlm.nih.gov/pubmed/20537515
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC159294/
[14] https://www.ncbi.nlm.nih.gov/pubmed/10761819
[15]https://www.researchgate.net/publication/274411047_Biomedically_relevant_chemical_constituents_of_Valeriana_officinalis
[16]https://www.researchgate.net/publication/250005457_Purification_Effects_of_Golden_Pothos_and_Peace_Lily_for_Indoor_Air-Pollutants_and_its_Application_to_a_Real_Environment
Research shows that as many as 20% of Americans use alcohol to help them fall asleep in the evening. Alcohol is a depressant, and it indeed induces sleep. However, it also contributes to poor quality shuteye, leading to interrupted snoozing, night sweats and disturbed REM sleep.
Think a nightcap may help you get a better night’s sleep? You are wrong!
Anyone who consumes alcohol from time to time knows that drinks like beer, wine, or spirits can leave you feeling drowsy. Due to this effect, many people started to use alcohol as a sleep aid. In fact, surveys show that as many as 20% of Americans use alcohol to help them fall asleep in the evening. Alcohol is a depressant, and it indeed induces sleep. However, it also contributes to poor quality shuteye, leading to interrupted snoozing, night sweats and disturbed REM sleep. [1]
Watch this video to learn what happens behind your closed eyes when you go to sleep after drinking.
Alcohol Doesn’t Aid Sleep
A study conducted in 2013 and published in Alcoholism: Clinical & Experimental Research has proven that alcohol doesn’t aid sleep.[2] Although it reduces the time required to fall asleep (sleep onset latency), it causes disrupted sleep in the second half of the night, by increasing non-REM sleep and reducing rapid eye movement.
Depending on the amount of alcohol you consumed, what seems like falling asleep will more likely be closer to passing out. Tolerance for the sedative effects of alcohol is quickly built, which means that over time you will have to drink more to enjoy the same sleep-inducing effects of alcohol consumption.[3]
Since alcohol is quickly metabolized, most people experience withdrawal symptoms in the second half of the night. Symptoms of withdrawal may include shallow sleep and multiple awakenings, REM rebound associated with nightmares or vivid dreams, sweating, and general activation.
Using alcohol as a sleep aid may not only lead to dependence, but also cause a variety of sleep problems such as sleepwalking, sleep talking, and sleep deprivation.
Lastly, alcohol also suppresses breathing and can precipitate sleep apnea. Since alcohol impairs sleep during the second half of the night, it reduces overall sleep time which leads to daytime somnolence.
The Relationship between Alcohol and Insomnia
Insomnia is often a chronic condition, and relying on alcohol to fall asleep will only make things worse and increase your risk of alcohol dependence. Alcoholism itself is associated with the complaints of poor sleep, increased sleep onset, sleep maintenance issues, and decreased delta and REM sleep.[4] Lastly, it increases the severity of obstructive sleep apnea, even in individuals without a history of OSA.[5]
How Does Alcohol Interrupt Sleep?
According to a study by Wayne State University and the National Institute on Alcohol Abuse and Alcoholism, after a few drinks, individuals report subjectively shallow sleep and frequent awakenings in the middle of the night.[6]
Research shows that, in the first half of the night, when the body is metabolizing alcohol, people spend more time in deep, slow-wave sleep and less time in REM sleep. REM sleep is a vital sleep stage for physical and mental restoration. This is why after a night of drinking, you wake up in the morning feeling drowsy and tired, no matter how long you stay in bed.
You probably think it’s great to spend more time in deep sleep, but it’s really not healthy for you. Why? Because our sleep architecture is biologically tuned to meet our body’s needs during sleep. Abrupt changes to our typical and natural structure of sleep aren’t generally good for our wellbeing.
During the second half of the night, sleep becomes even more disrupted. As alcohol is metabolized and its sedative effects start to disappear, the body goes through a process the experts call a rebound effect[7]. The rebound effect includes a sudden change from deeper to lighter sleep, with more frequent awakenings during the second half of the night. The abrupt frequent awakenings can manifest as micro-awakenings that you don’t even remember, but they still interrupt the natural flow of sleep and its quality. Our sleep architecture shifts again, and we spent significantly less time in slow wave sleep. The rebound effect may also include more time in REM sleep, which is characterized by vivid dreaming. Disrupted REM sleep also Increases risk for parasomnias including sleepwalking and sleep eating.[8]
Mid-night awakenings after drinking are common because alcohol affects the normal production of chemicals in the body that induce sleep (such as melatonin and ATP) when you’ve been awake for a long time, and recede once you’ve had enough rest. After drinking, production of adenosine (vital for inducing sleep) is increased, allowing for a fast onset of sleep. But it recedes as quickly as it came, making you more likely to wake up before you’re truly rested, and preventing you from falling asleep again – another consequence of the rebound effect.
Simply explained, alcohol’s adenosine-boosting effects mess up with your internal sleep drive and make you sleep at times other than you would naturally, throwing your natural sleep-wake cycle off course.[9]
This is the primary way alcohol disrupts sleep, but the effects of going to sleep with alcohol in your system don’t stop here. Here are other ways how alcohol interrupts nightly rest.
Disrupted sleep-wake cycles
Alcohol suppresses melatonin, the primary regulator of sleep-wake cycles. Research shows that a moderate dose of alcohol just 1h before bedtime can decrease melatonin production by 20%.[10] Alcohol reduces the ability of the master biological clock to respond to the light which helps it to stay in sync with the 24h day/night cycle.[11]
Effects on circadian rhythm
Let’s quickly refresh our knowledge on the importance of the body’s internal clock. Our 24-hour rhythms are managed by the master biological clock which is responsible for coordinating circadian rhythm activity through the body.
Circadian rhythms are crucial for our health because they regulate nearly all of the body’s processes, from metabolism and sleep to immunity, energy, our sexual drive, cognitive functions, and mood. Alcohol disrupts circadian functioning and directly interferes with the ability of the master biological clock to synchronize itself. Since our internal clock is, as we previously mentioned, responsible for regulating all of the major body’s processes, the disruptive effects of alcohol can be widespread, affecting not only our sleep, but other systems as well, resulting in poor liver function, leaky gut, and depression.
- Poor liver function – Our liver is the body’s filtering system, and its primary role is to metabolize food and chemicals (including alcohol) and to remove toxins from the bloodstream. When alcohol disrupts the circadian rhythms regulating the liver, it compromises liver function and contributes to liver toxicity and disease.
- Leaky gut – The gut and its microbiome are often referred to by experts as the body’s second brain, and it’s also operated by circadian rhythm activity. When thrown out of sync, the lining of the gastrointestinal tract becomes more susceptible to permeation, meaning the lining of the GI tract is more likely to allow bacteria, and toxins to leave the intestines and enter the bloodstream.
- Depression – There’s a complicated relationship between depression, alcohol, and sleep. Depression and insomnia are often comorbid, and even the presence of moderate amounts of alcohol may make things even worse, especially when it comes to further pushing your circadian rhythm out of sync.
Diuretic effect
Your body knows that nighttime is time for sleep, and not adequate time for trips to the bathroom. Simply explained, your body has learned to put your bladder into hibernation for the night. But alcohol, since it has a diuretic effect, will cause you to wake up to use the restroom during the night, and interrupt your sleep.
Night sweats
Drinking affects your sleep homeostasis by messing up with the body’s core temperature. Alcohol first cools you down, helping you to fall asleep, but in the second half of the night, your body temperature will rise. Due to alcohol’s diuretic effect, your body will be encouraged to lose the extra heat through sweat, ultimately making you dehydrated. Night sweats may be particularly problematic for people who already sleep hot. However, once the effects wear off, your body counteracts it with a corresponding rise in temperature, causing night sweats and making you wake up earlier than expected.
Snoring and sleep apnea
Alcohol relaxes all the muscles in your body, which means that the relaxed tissue in your throat, mouth, and nose may stop proper air flowing, causing the air to vibrate, and resulting in loud snoring.
Effect on sleep disorders
Research shows that alcohol consumption may lead to the development of new sleep disorders or make existing ones worse, particularly when it comes to insomnia[12] and OSA (obstructive sleep apnea).[13]
As you can see, alcohol can equal a fitful night’s sleep. Sleep and circadian rhythm interference from alcohol contribute to next-day sleepiness, fatigue, irritability, and difficulty focusing. Even if you don’t experience it as a typical hangover, alcohol-related sleep loss negatively affects your mood and performance during the day.
The Bottom Line
The bottom line is that the more you drink, and the closer it is to your bedtime, the more it negatively affects your sleep. It doesn’t matter if you take moderate amounts of alcohol at bedtime. Almost any quantity can alter your sleep architecture and natural sleep flow.
Alcohol may severely affect your sleep, but that doesn’t mean you should stop consuming it completely. So, you may be wondering how much alcohol is too much for sleep?
Ideally, you should drink 2 to 3 times a week. This gives you enough room to enjoy a glass of fine wine at your favorite restaurant, an evening cocktail with your friends, and a cold beer at home after a busy week – without interfering with healthy sleep.
And when is the best time to consume alcohol?
Circadian rhythms affect how the body responds to alcohol, depending on the timing of alcohol intake. Research shows the body metabolizes alcohol differently at different times of the day. Your body is least prepared to process alcohol in the morning, and best metabolized early to middle evening hours – or during the traditional “happy hour” time.
Resources and references
[1] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4666864/
[2] https://onlinelibrary.wiley.com/journal/15300277
[3] https://pubs.niaaa.nih.gov/publications/arh25-2/101-109.htm
[4] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2775419/
[5] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5840512/
[6] http://grandchallengesforsocialwork.org/wp-content/uploads/2015/12/WP14-with-cover.pdf
[7] https://en.wikipedia.org/wiki/REM_rebound
[8] https://pubs.niaaa.nih.gov/publications/arh25-2/101-109.htm
[9] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5821259/
[10]https://www.researchgate.net/publication/291450048_An_interaction_of_melatonin_with_alcohol_A_case_study
[11] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2778757/
While one pillow is often enough, in some cases, it’s worth sleeping with two pillows. If you are a side sleeper, sleep with one pillow under your head and with one pillow in between your knees. If you are a back sleeper, place a pillow under your knees.
Heading to a new place and in search of fresh bedding? Struggling to find a pillow that doesn’t leave you with neck discomfort, regardless of your efforts? You’re in good company. Research through randomized trials shows that 15 to 20% of adults globally suffer from discomfort in their arms, backs, and necks, or experience stiffness regularly each week. While for some, it may only be a sporadic annoyance, there are those who face undefined pain nearly every day.
Even if you are merely bored with your old bed, navigating the market can be hard enough. With the current offer of endless materials, mattress configurations, even sheet prints, you may find yourself feeling overwhelmed and confused. Knowing which of these things will suit you takes some trial-and-error time until you start to feel comfortable and confident in making a decision.
In these situations, it is helpful to remind yourself how many of these items you need for optimal sleep. When it comes to pillows, the fact is that most people require only one, though it needs to be of good quality and tick a few customized boxes. However, there are scenarios in which you might need an extra pillow or two (and not for décor purposes), or even prefer to sleep without any at all. Several factors may influence this decision, and we’re just about to unpack them.
The Main Pillow
Whether or not you need more than one pillow, or whether the one you already have suits you, it all depends how you feel sleeping on it. Do you get enough rest? Do you wake up without numbness or pain? Do you feel refreshed and energized in the morning? These are some goals to strive for when it comes to your bedding. The right setting should keep your spine perfectly aligned, which means no head tilting or neck strain. To achieve this state, your pillow’s loft has to be high enough to prevent your head from sinking too deep, but low enough not to push it too far in the other direction. Typically, you will come across three categories addressing the loft: low (up to three inches high), medium (between three and five inches), and high loft (five inches and above).
The material should be not only comfortable but also hypoallergenic, in case you’re one of the people whose allergies act up around bedtime. Moreover, the density of the pillow needs to meet your needs – softer or firmer, with the surface flatter or shaped. This will determine how deep your head will sink and whether the material will conform around it for additional, corrective support. Lastly, the breathability of your pillow can mean the difference between healthy rest and disrupted, poor quality sleep, especially for those who tend to sleep hot. Excessive heat can be trapped inside the pores of high-density materials such as memory foam and cause much distress for the sleeper.
However, when your pillow doesn’t already meet all or most of the criteria just mentioned, and you wake up sweating or tired, it’s time to make a change. Figuring out exactly which features will do the trick for you starts with the way your body is positioned during the biggest portion of the night.
Sleep Positions
Which way you face during sleep classifies you as a side, stomach, or back sleeper. Each of them come with many variations that have unique benefits and downsides and therefore require different levels of support.
Side Sleeping
Side sleeping is considered the best option out of the three. The way your organs are positioned when sleeping on your side means you’ll face the smallest chances of discomfort – this state is known to prevent sleep apnea, acid reflux, and snoring. Here are the three most common ways people settle down on their side:
- Fetal position – legs are bent in the knees and arms are in the front or under the pillow.
- Log position – both arms and legs are stretched out and you look as if you were standing upright.
- Yearner position – legs are stretched out, but arms are reaching forwards.
An adequate amount of support means different things between the three categories, but sleeping on your side makes the least room for issues. The only thing to be concerned about here is the loft of your pillow – side sleepers require higher profile, supportive surfaces to keep their head in line with the spine. Memory foam does a great job of keeping everything in place as it usually has excellent conforming properties – unless you can’t handle the heat, that is. In essence, any cushion that is on the thicker end, and keeps your head straight will do the trick, but make sure it’s comfortable.
Back Sleeping
This position can work well in certain circumstances, but not everybody will benefit from it. Acid reflux prevention, proper spine alignment, and even weight distribution across your body are some of the upsides that come with sleeping on your back. Unfortunately, facing upwards isn’t the best idea if you have sleep apnea or tend to snore, as back sleeping is known to worsen these conditions, directly impairing the efficiency as well as the duration of your rest.
Back sleepers take up about 13% of the total population. They commonly spend their nights in these positions:
- Savasana – facing the ceiling, arms, and legs straightened out as if standing upright.
- Soldier – same as Savasana except with one leg bent at the knee.
- Starfish – legs stretched, arms above the head.
When you lay down in this manner, there are a few things to be addressed. First, your main pillow needs to have a lower medium loft and preferably some contouring properties, filling out the empty bit of space below your neck. A good option for this would be a pillow with a divot.
Stomach Sleeping
Officially the worst option out of the three, sleeping on your stomach does come with some pros – it prevents snoring and sleep apnea. Unfortunately, the list ends there, as the downsides to this way of sleeping take over. When you sleep on your stomach, your entire weight distributes around your core and presses your organs into the bed. Besides decreasing their ability to expand and impairing the way they function, this also creates a great deal of stress in your ankles and wrists as they are left to handle your body’s pull. Furthermore, stomach sleeping causes even more wrinkling and breast sag than side sleeping. The discomfort caused by this position makes stomach sleepers toss and turn noticeably more often than other types of sleepers, reducing the quality of their sleep.
Finally, this position is a bad idea if you experience back or neck pain, as your spine is likely to be curved, especially if you use a thick pillow or have a very soft bed. In fact, stomach sleepers are the only group that would benefit from sleeping without a pillow altogether. If this notion is too strange for you, using a thinner but moldable pillow would be optimal, as it would allow you to turn around as much as you need to without sacrificing your comfort.
Common Types of Pillows
By now, you’ve hopefully got a picture of what you should be looking for. To give you a bit more insight into whether a model type may suit you or not, let’s take a look at the general characteristics of the ones most commonly found on the market.
Memory foam is an overall good pick for corrective purposes. This material molds around your head and neck, filling all gaps and leaving no room for bad posture. The surface of most models is around medium firm, as it’s meant to prevent you from sinking in too deep. The flaws of memory foam stem from its high density. If you are someone who struggles with excessive heat during the night, this material would be a bad idea as it’s compact structure leaves little room for air to circulate. Additionally, if you like those pillows that feel supple and soft at first touch, the memory foam surface might feel a bit awkward and hard at first, as it takes some time before it molds around you. Overall, memory foam is a widespread favorite and recommended for people who experience neck pain or headaches.
Latex is known for its soft feel and long lifespan. Highly responsive and mold resistant, this type of cushion is also eco-friendly. According to this trial, latex is deemed most helpful for dealing with persistent headaches and arm pain upon waking. However, latex definitely doesn’t sleep the coolest of the lot and can be pricey, especially the organic models. Before you decide to give it a go, make sure you aren’t allergic.
Gel-infused pillows are made for hot sleepers. Cooling property is their main selling point, along with being hypoallergenic. Even some memory foam models are infused with gel for this reason, but that usually gives them the “average” instead of “heat-trap” status in this area.
Feather pillows have been used for quite a while. They are famous for their light weight, softness, immediate responsiveness, and admirable durability. Like all other models, though, they have their cons. For one, they aren’t very breathable, disqualifying them for hot sleepers. Further, the feathers can poke through the fabric, causing skin irritation even for people who aren’t allergic. Lastly, those whose allergies act up at nighttime, as well as those who are allergic to feathers – better look at other options.
Contour pillows curve down in the middle part (think: headrests on a massage bed, except not empty in the center) and considered suitable for side and back sleepers. They are very supportive, promote good posture, and help reduce snoring.
When One Pillow Isn’t Enough
As mentioned above, most issues with pressure points and pain can be prevented or decreased to an extent by purchasing a suitable pillow. However, there are times when an extra mile is necessary.
Every one of these positions has a pressure point or two besides the one around the neck area. Your mattress would preferably address these, but if this isn’t the case and you can’t replace it, or you simply require sturdier support, additional pillows come in handy.
Side sleepers: to decrease the stress on your hips, professionals sometimes recommend placing another, thin pillow between your knees, or getting a body pillow that can be used in a similar manner. The goal here is to keep your pelvis straight. If you experience chronic pain in the lumbar area despite doing everything right, you may also put a thin layer below the knees or ribs.
The lumbar region is the back sleepers’ main pressure point. You can elevate most of the discomfort by putting a thin pillow under your knees, prompting your back to sink more deeply into the surface of your bed and filling the awkward gap between.
For stomach sleepers, a thin cushion placed under your hips may be of additional help in reducing the pressure in your muscles and joints caused by sinking too deep into the mattress.
Pregnant sleepers often need plenty of support, too. As the stomach grows, new pains and uncomfortable stretches create much distress to the expecting mother. For this reason, doctors frequently advise using a body pillow to hug around, which will ensure the stomach is adequately supported. Fixing up extra pillows behind the back, between or under the knees is also not rare. Just try not to pile up a bunch of thin pillows on top of one another, and instead opt for one pillow per area. You may think there is no difference, as the height is the same, but that may do more harm than good. By picking one over many, you decrease the possibility of one cushion sliding out or falling off the bed.
Body Pillows
This oversized cushion, although used mainly by pregnant people, may benefit pretty much everyone who is looking for a whole-body support system in the bed. There are two common types of body pillows: the U-shaped, meant for side and back sleepers alike, and the I-shaped one indicated only for side sleepers. Not convinced? Here are some features that prove body pillows are worth a shot:
- Relief from pain in critical points – if you put one leg over, hip stress is taken care of. Hug it with your arm and ensure the shoulders and elbows are relaxed, too.
- Decreased tossing and turning. The U-shaped ones, in particular, are designed to lock you in place comfortably, helping you fall and stay asleep.
- Decreased snoring. By preventing you from turning over to your back during sleep, this cushion will stop you from snoring as well.
- Relief from neck or back pain. Having something to lean over ensures your muscles won’t need to be tense to keep you in place, minimizing chances of numbness or pain the next morning.
- Stress relief. A body pillow is essentially a grown-up version of a teddy bear. Not only will holding onto it make you feel more safe and secure, but your brain will associate the two and start releasing oxytocin, a hormone that reduces stress.
Knee Pillows
Although we have mentioned the possibility of placing a thin layer between or under your knees, there are specialty items made precisely for this purpose. Most knee pillows are hourglass-shaped, which promises they won’t slip away during your sleep. They are meant to relieve any aches and discomfort that you may feel while sleeping on your sides, such as tension in your calves or hips. They also suit people who want to prevent the contact between their legs – a reasonable request, especially during summer or for those with skin issues.
Although placing it between their knees may not be beneficial or even practical for them, back sleepers who struggle with slow circulation can put a wedge-shaped knee pillow under their legs instead and promote healthier blood flow. Pregnant women could use the support when back or pelvis issues arise, but also as a measure to prevent such difficulties in the first place.
Lastly, people with chronic pain, injured individuals, and those with restless leg syndrome (RLS) may find comfort in using a knee pillow. As RLS causes tension and pain in one’s legs, and can make them shake for hours during sleep, some knee pillows are specially designed with straps that can be tied around the legs and decrease excessive movements. Besides aiding the person with RLS, this is also helpful if they sleep with a partner, as a precaution against being kicked during sleep.
Wedge Pillows
These cushions come with a tapered incline, intended to slightly lift up your head, legs, torso, or any other area you may need them for. They are usually on the firm end, meant to use alongside your regular pillow and not instead of it. A wedge pillow can be handy for plenty of scenarios: as back support while watching TV or resting on your sofa, as an elevated headrest to prevent acid reflux, a platform for your legs to promote blood circulation, etc.
A wedge pillow can come as a single piece or have multiple parts. Highly customizable and sturdy, these products can vary in almost every aspect and suit a broad audience of customers. Here are some reasons you may want to consider buying one for yourself:
- Conforms closely to your body
- Convenient and comfortable
- Prevents varicose veins
- Decreases snoring
- Promotes better blood and air flow
- Helps with acid reflux